ABSTRACT
INTRODUCTION
According to the Joint National Committee, hypertension can be defined as systolic BP level of ≥140 mmHg and/or diastolic BP level ≥ 90 mmHg.1 Hypertension is an important modifiable risk factor for Cardiovascular Diseases (CVD), making it one of the significant contributors of premature death and morbidity.2 Rarely accompanied by symptoms, it is generally identified while seeking medical care for any unrelated problem. People with hypertension have complaints of headache at back of the head, vertigo, lightheadedness, tinnitus, blurred vision, sweating, facial flushing and palpitations. Uncontrolled or poor management of hypertension results in serious complications like coronary heart disease, cerebrovascular disease, vision loss, peripheral arterial disease and renal insufficiency. Lifestyle factors that elevate the risk of high blood pressure includes stress, obesity, smoking, alcohol consumption, physical inactivity and excess salt intake in diet. For better management of hypertension and to abate the risk of cardiovascular disease or complication, lifestyle changes are recommended before initiating drug therapy. Lifestyle changes involves reduction in weight, decrease salt intake, increase in potassium rich food like banana, physical activity for at least half an hour per day, low fat diary food, reduce alcohol consumption and a healthy diet. Blood pressure medications are used when lifestyle changes are inadequate to control BP.3 Anti-hypertensive are class of drugs that are used to control hypertension. Various antihypertensive medications that control blood pressure by one or the other means includes diuretics, ACE inhibitors, ARBs, beta blockers, calcium channel blockers, alpha adrenergic blockers, vasodilators, and RAS antagonist.4
Between 2000 and 2025, it is expected that the number of persons with hypertension will increase globally. This is due to the fact that more than 80% of the world’s population is regarded as developing, the worldwide population is ageing and expanding, and blood pressure rises with age globally. Until now, development has been linked to increasing exposure to the major environmental factors that contribute to high blood pressure, including as consuming too much salt, calories and alcohol.5 Idiopathic pathophysiologic etiology causes high blood pressure in around 90% of patients, and is referred to as essential hypertension. Only about 10% of people suffer secondary hypertension, which is caused by a co-morbid disease or a pharmacological side effect.1 Hypertension is one of the leading causes of death and disability in many countries and its prevalence is rising swiftly. In developed countries, hypertension is the seventh major cause of mortality, while it is the fourth leading cause in poor nations.6 According to recent studies, almost 1 billion adults (about a quarter of the world’s population) suffer with hypertension, with the number expected to rise to 1.56 billion by 2025.7 In India, 20-40% of adult hypertension patients live in cities, while 12-17% lives in rural areas. India is home to 15% of the world’s uncontrolled hypertension sufferers.8
WHO has defined Quality of Life (QOL) as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns”. Health Related Quality of Life (HRQOL) addresses health-related domains that are impacted by elements such as physical, psychological, social, and environmental aspects.2 The assessment of hypertension patients’ quality of life is crucial. QOL is important to patients, physicians, and policymakers, and interest in HRQOL has risen significantly in recent years.9 It involves more than direct measures of health, life expectancy, including causes of death and focuses on the impact of the patient’s health status on his quality of life. It appraises both the positive and negative aspect of life. A number of instruments can be used to measure quality of life, in this study however; the SF-12 questionnaire was used because it has been found to be reliable, cost effective and easy to complete.10 Function and well-being may be more important to people with chronic diseases than the physiologic indicators that clinicians find useful.11 Hypertensive patients, like patients with other chronic medical problems, are subjected to a wide range of intense emotions, which raises their risk of mental health issues, including anxiety and sadness.12 Furthermore, psychosocial factors can have an impact on health outcomes; self-reported health status has been found to be a stronger predictor of mortality and morbidity than many objective health indicators.13 Blood pressure, organ damage, co-morbidities, and medication all affect hypertension patients’ quality of life.14
World Health Organization with help of 15 collaborating factors around the globe constructed two tools for estimating quality of life of patients (WHOQOL-100 and WHOQOL-BREF). WHOQOL-100 consists of 100 questions that cover following dimension; physical health, level of independence, environmental, social and religious/spiritual/ personal belief. The WHOQOL-BREF questionnaire is a brief style of WHOQOL-100 is a cross cultural instrument that can cover broadly all features of quality of life including physical health, social, physiological and environmental. This psychometric tool was developed in year 1992. As WHOQOL-BREF doesn’t impose any burden on the patient, so it can be useful instrument to assess HRQOL.15
Overall goal of the present study includes the effect of physical and psychological factors on health-related quality of life of hypertensive patient. The current study includes the various socio-demographic characterization, WHO HRQOL BREF questionnaire, types of medication and their side effects as well as to identify risk factors and associations of insufficient knowledge on hypertensive patients. This research will allow health care providers to include socially and culturally acceptable quality of life education programmes for hypertensive patients.
MATERIALS AND METHODS
Study Site
Hospital based observational study was carried out after being approved by ethical committee, this hospital based observational study was carried out in medicine ward and out-patient department of a tertiary care hospital, Haryana, India. The institutional ethics committee gave its approval to the trial protocol in November 2021 (Project Number: IEC 2121). Each respondent gave their informed consent to conduct the interview, and confidentiality and privacy were maintained. To protect confidentiality, respondents’ names were replaced on the questionnaire with serial numbers, and this was done throughout the study and even after it was over. Respondents’ serial numbers rather than names were put on the questionnaire to ensure secrecy. In addition, respondents were informed that refusal to participate in the study or withdrawal from it would not result in any loss of benefits or penalty. No patient was deprived of standard treatment during the duration study.
Study Participants
From the general medicine wards of OPD and IPD, 300 patients who had been diagnosed with hypertension by the doctors had been gathered. The sample size was calculated using the formula n=4PQ/d2, where P, Q, and d represent prevalence, 100-P, and 20% of P, respectively. The prevalence rate was derived from a study conducted by Parkash. et al. and Narang S. et al.16,17 The inclusion and exclusion criteria for the study will be evaluated for each subject. Patients are deemed hypertensive if their blood pressure is greater than 140/90 mmHg. All the patients were made aware about all the aspects and the purpose of the study in their native language prior to recruitment. Informed consent of the patients or their representative were taken by signing informed consent form. The study uses WHOQOL-BREF questionnaire that were marked by patients or their representative. Duration of the study was six months.
Patients with a diagnosis of hypertension, blood pressure greater than 140/90 mm Hg, who are both male and female, who are able and willing to give a written consent for information, who have had the condition for more than 3 years, and who are at least 30 years old were included in the study. Patients below 30 years age, those with abnormal mental status, pregnant women, nursing mothers, hypertensive patients with normal blood pressure, patients with tuberculosis, patients with Vitamin deficiencies, patients receiving steroid therapy, patients with disabilities were excluded in the study.
Study Tools
The patient’s blood pressure was measured using a sphygmomanometer and stethoscope. The World Health Organization’s WHOQOL-BREF questionnaire was used to evaluate the health-related quality of life of hypertension patients. Patients were questioned about their QOL using the WHOQOL-BREF questionnaires.18 Out of four domains, domains assessed were physical (pain and discomfort, activity of daily living, mobility, sleep and rest, work capacity and dependence on medicinal substances and medical aids energy and fatigue) and psychological (bodily image and appearance, negative feelings, positive feelings, self-esteem, spirituality / religion / personal beliefs, thinking, learning, memory and concentration).
RESULTS
This study was carried out to access the hypertensive patients in view for analysis of QOL and its determinants. A total 300 patients diagnosed with hypertension were recruited, they met our exclusion and inclusion criteria. All of the participant in this study were signed with a written consent form during the study. A Case Report Form (CRF) was designed that include all the participant characteristic, demographic details, socio-demographic details, laboratory findings, social and family history, past and present medical history, life style modification as shown in Tables 1 and 2.
| Mean | P-value | |||
|---|---|---|---|---|
| Variables | Physical | Psychological | SD | |
| Gender | ||||
| Female | 3.2143 | 3.6532 | 3.00763 | |
| Male | 3.9123 | 3.9953 | 3.6527 | 0.29629 |
| Age (year) | ||||
| 30-39 | 3.8721 | 3.9543 | 3.6511 | |
| 40-49 | 3.6026 | 3.4591 | 3.2237 | 0.29916 |
| 50-59 | 3.7043 | 3.9287 | 3.6345 | |
| 60-69 | 2.9729 | 3.0726 | 3.1310 | |
| 70-79 | 2.6847 | 3.2217 | 3.6392 | |
| Area | ||||
| Rural | 3.6512 | 3.8736 | 3.3371 | |
| Urban | 3.4352 | 3.86871 | 3.4562 | 0.36868 |
| Sub-Urban | 3.2271 | 2.9437 | 3.5381 | |
| Education | ||||
| None | 3.6545 | 3.5423 | 3.8654 | |
| Primary | 3.8667 | 3.8645 | 3.9757 | 0.3557 |
| Secondary | 4.0764 | 4.3423 | 3.8656 | |
| University | 4.1254 | 4.3213 | 3.2352 | |
| Pharmacotherapy | ||||
| Single | 3.3443 | 3.2345 | 3.5642 | |
| Combination | 3.4123 | 3.2134 | 3.3345 | 0.31306 |
| Triple-Combination | 3.9342 | 3.8743 | 3.6874 | |
| Types of Medications Used | M | F | Number (N) | Percentage (%) |
|---|---|---|---|---|
| No Medications | 15 | 6 | 21 | 7% |
| Single | 72 | 54 | 126 | 42% |
| Double-Combination | 75 | 36 | 111 | 37% |
| Triple-Combination | 27 | 15 | 42 | 14% |
| Side-Effect | ||||
| Yes | 27 | 36 | 63 | 21% |
| No | 93 | 144 | 237 | 79% |
| Types of Side-Effect | ||||
| Nausea | 06 | 09 | 15 | 5% |
| Vomiting | 03 | 03 | 03 | 1% |
| Cough | 15 | 06 | 21 | 7% |
| Any other | 15 | 09 | 24 | 8% |
| Sl. No | Questions | MEAN (300) | SD (±) |
|---|---|---|---|
| Physical Domain Question | |||
| 1 | To what extent do you feel that physical pain prevents you doing what you need to do? | 2.85 | 0.988 |
| 2 | How much do you need any medical treatment to function in your daily life? | 3.15 | 0.954 |
| 3 | Do you have enough energy for everyday life? | 3.17 | 0.943 |
| 4 | How well are you able to get around? | 3.44 | 1.047 |
| 5 | How satisfied are you with your sleep? | 3.51 | 0.846 |
| 6 | How satisfied are you with your ability to perform your daily living activities? | 3.33 | 0.829 |
| 7 | How satisfied are you with your capacity of work? | 3.41 | 0.954 |
| Psychological Domain Question | |||
| 8 | How much do you enjoy life? | 3.39 | 0.973 |
| 9 | To what extent do you feel your life to be meaningful? | 3.48 | 0.904 |
| 10 | How well are you able to concentrate? | 3.21 | 0.977 |
| 11 | Are you able to accept your bodily appearance? | 3.28 | 0.865 |
| 12 | How satisfied are you with yourself? | 3.67 | 0.964 |
| 13 | How often do you have negative felling such as blue mood, anxiety. ..depression? | 2.14 | 0.841 |
| 14 | Physical Domain Score | 56.625 | 0.2274 |
| 15 | Psychological Domain Score | 54.875 | 0.5413 |
Various parameters of socio-demographic parameter have represented in Table 4. According to our finding rate of hypertensive patients were observed in female population (60%) when compared to male population (40%). Data suggest that a greater number of patients were in age group between 60-69 (34%). Least number of patients were observed in the age group 30-30 (10%), 70-79 (12%), 80-89 (5%). Out of total enrolled patients, 44% patients resided in rural area while 56% of patients were from urban area where and data also shows that the highest number 37% and 20% of subject have received primary and secondary education respectively. 36% of total patients were found to be uneducated. Discussing about the lifestyles of patients 111 (37%) of females were housewife, 75 (25%) were employed, 30 (10%), 3(1%), 21 (7%) were pensioner, government service retired and service retired. Least number of 9 (3%) subjected were involved in their own business. Overall study shows that majority of the patients are females, between the ages of 60-69 years, most of them have primary education and are engaged in other forms of employment as business and service also some of them are retired and full-time housewives.
| Parameter (Range) | Value (N) | ||
|---|---|---|---|
| Gender | |||
| Male | 120(40%) | ||
| Female | 180(60%) | ||
| Area | |||
| Rural | 46% | ||
| Urban | 54% | ||
| Occupation | |||
| Businessman | 9 (3%) | ||
| Employed | 75 (25%) | ||
| Unemployed | 51 (17%) | ||
| Housewife | 111 (37%) | ||
| Pension | 30 (10%) | ||
| Government Retired | 3 (1%) | ||
| Service Retired | 21 (7%) | ||
| Age | |||
| Gender | Male | Female | % |
| 30-39 | 12 | 18 | 10 |
| 40-49 | 12 | 33 | 15 |
| 50-59 | 21 | 51 | 24 |
| 60-69 | 42 | 60 | 34 |
| 70-79 | 18 | 18 | 12 |
| 80-89 | 9 | 6 | 5 |
| Level of Education | |||
| Gender | Male | Female | % |
| None | 30 | 78 | 36 |
| Primary | 54 | 57 | 37 |
| Secondary | 27 | 33 | 20 |
| University | 15 | 6 | 7 |
Table 2 explain the medication used by hypertensive patients and their possible side effects they suffered. Hypertensive medication is widely used to control the blood pressured where various class of drugs are available now a days. Comparing all the hypertensive drugs, 126 (42%), 111 (37%), 42 (14%) had received single, double combination and tripe combination of medication. Least number of 21 (7%) patients haven’t required any medication. Out of total population 237 (79%) haven’t reported any possible side effect where 63 (21%) had reported their side effects. Overall analyzing the reported side effects majority of patients 15 (5%), 3 (1%) and 21 (7%) have nausea, vomiting and cough respectively. Rest of them around 8% of had other.
Both physical and psychological factors questionnaire response are represented in graphical bar diagram as shown in Figure 1. Out to total 13 question Q1-Q7 belongs to physical factor and Q8-Q13 belongs to psychological factor. Physical domain-based questionnaire that asks about pain and discomfort, everyday activities, mobility, sleep and rest, work capability, dependence on drugs and medical devices, energy, and weariness. 28% of people felt that physical pain prevents their life from doings and 41% of patients are able to get around good amount. Also, higher in patients about 38%, and 60% of patients had energy for their everyday life, able to get around good amount and patients were satisfied with their sleep, while 41% of patients can only move about easily but are not comfortable with their sleep. Less than 5% of patients require medical care in order to carry out their daily activities. Approximately 43% of people are content with their capability for doing activities of daily living, and 41% are content with their capacity for employment. Based on a psychological domain, the questionnaire asks about self-esteem, body image and appearance, negative and positive moods, spirituality, religion, and personal views, as well as thinking, learning, memory, and attention. In comparison to 14% of patients who felt their lives were fully meaningful and 7% of patients who were able to focus intensely, 1% of patients reported experiencing immense joy in life. Also, 36% of total patients completely accepted their bodily appearance and 22%-23% of total patients were very satisfied and had no negative felling such as anxiety, depression, blue mood as shown on Figure 1.
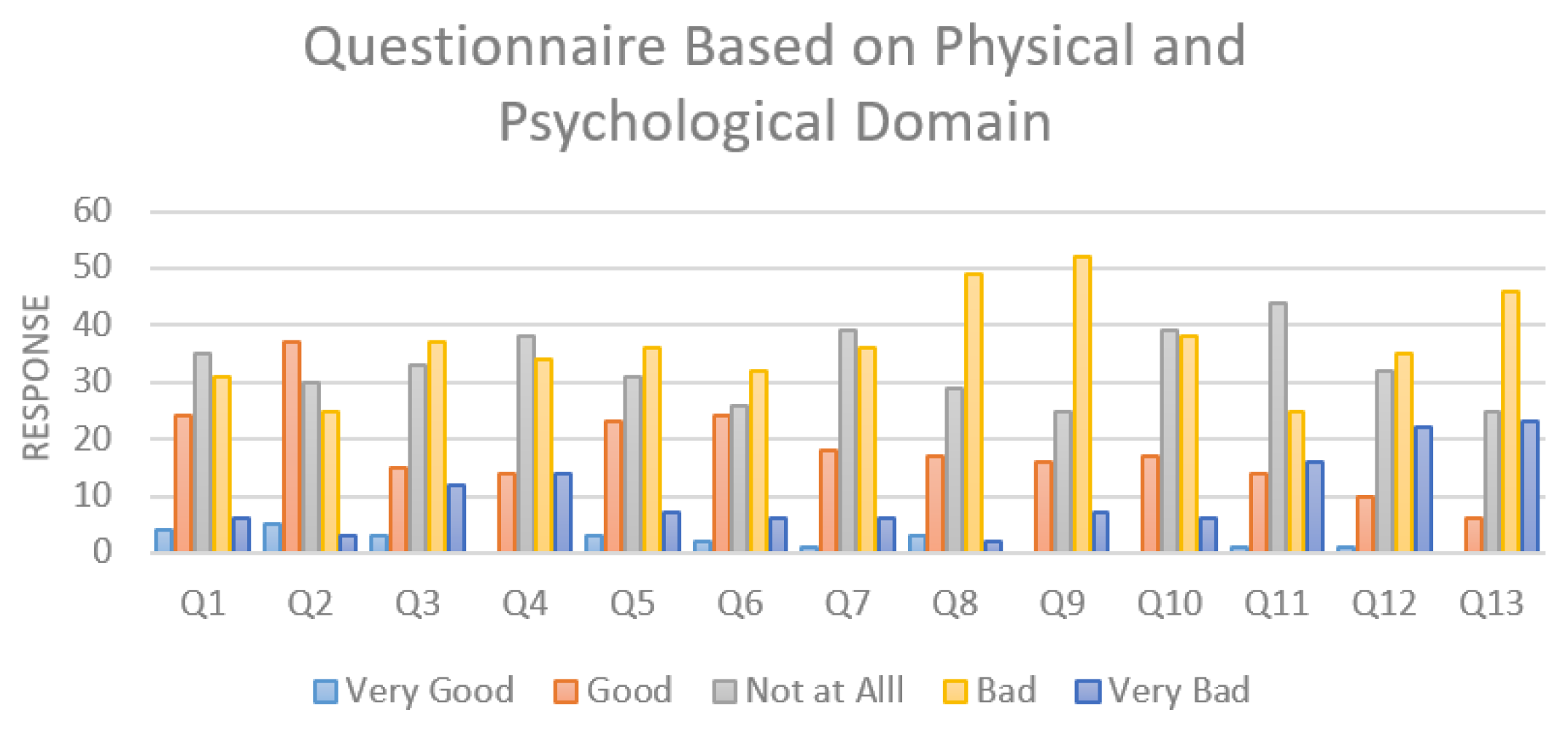
Figure 1.
Questionnaire Based Response on Physical and Psychological Domain.
A quality based designed survey that include two domains (physical and psychological) and all the finding are elaborated in Table 3. Figure 1 elaborate the order of response by the respondents from WHOQOL-BREF scale questionnaire as very bad, bad, moderate, good and very good. Our result shows higher majority of very bad as well as bad response which indicate that population in that particular area have very poor quality of life and fewer population have very low good response which shows very few people in that area have good quality of life.
DISCUSSION
Hypertension is considered as major public health challenge across worldwide. Globally, one third of population suffer from hypertension and their associated diseases and half of the total death were caused by cardiovascular diseases and cardiovascular accidents due to higher prevalence of hypertension. Hypertension is also linked as most important predisposing factor for cardiovascular diseases and affect quality of life.3 Overall total 322 case studies, we found 7 patients were not able to communicate and 6 subjects couldn’t respond correctly also 9 patients get reverse back during the study. Among 300 study respondents, Table 4 shows that, prevalence of female was more as compared to male. Person from age group 60-69 years were more susceptible to hypertension. The majority of patients (38%) are from urban areas, and the majority of study participants (37%) have only completed their first year of education. Fewer than 7% of individuals had finished their higher education. 14% of the patients were taking three different medications at once, while 49% and 37% of the patients were receiving single or combination therapy. When compared to the male population, our study found that females were more likely to have hypertension. Similar prevalence of hypertension among females was documented in the study by Bhavit Oza et al.19 High incidence in females may be associated with a drop in estrogen production after the age of 40, which could cause arteriosclerosis.20,21
According to our study it shows that classes and number of anti-hypertensive medication prescribed had no any influence on quality of life among the study participants as shown in Table 2. Various clinical trials required to identify the superior antihypertensive medication over another in controlling blood pressure without impairing the health-related quality of life. In a study conducted by Mclness GT et al. and Saini et al. pointed out that the aggressive treatment plans with single or combination therapy does not impaired quality of life but other various studies shows role of drugs and their possible side effect.3
Age, education level, self-management efficacy and health literacy were all related to the HRQOL of patient with hypertension, which means that patients who are more elderly and have lower education level, low self-management efficacy and poor health literacy get worse HRQOL. This may imply the necessary to introduce routine assessment of health literacy and self-management efficacy into assessment procedures for hypertensive patients’ health management. An assessment concluded by Chenli Wang et al. explained the various parameter that can help professionals to identify the population at greatest risk for poor health outcomes and low well-being in the future. Also, effective interventions such as direct guidance and education to raise the self-management efficacy and enhance health literacy might improve the HRQOL of patients with hypertension.22
In our study findings, the prevalence of the hypertension was found in females comparing to males and majority of them were belonging to lower economic status. Health intervention strategies need to be further explored and adapted to the context of improving HRQOL for patients who suffer from hypertension and other chronic non-communicable diseases. According to Meng Xiao et al. showed perceived economic burden caused by hypertension was the most common factor impacting on patients’ HRQOL. Female patients were more susceptible when compared to male patients.20
The World Health Organization’s Quality of Life Group created the WHOQOL-BREF, a 26-question survey. It is a condensed version of WHOQOL-BREF. The scale utilized is a five-point liker-type scale, with a score ranging from one to five, with one being the worst level and five being the best.23 A standard tool that has been used to evaluate quality of life in a number of chronic conditions is the SF-36 scale. It is available in many different languages.24 It may be assumed that the SF-36 questionnaire is less sensitive to detect and assess health characteristics unique to hypertension because of the reduced declines in several HRQOL indicators in hypertension compared to various other chronic conditions. These traits include symptoms including headache, dizziness, irritability, memory loss, blurred vision, sexual dysfunction, difficulties sleeping, and mental health problems like anxiety and melancholy.25
On other hand, various questionnaire responses were analyzed through the mean and standard deviation responded from the patient’s data. The average response rate on the WHOQOL-BREF questionnaire is summarized in Table 3. It was discovered that the physical domain’s mean score was higher than the psychological domain’s [56.623 ± 0.2274) and 54.875 ± 0.5413), respectively], the result we found from our study was similar to the result of study done in rural North of Vietnam, Iran, Nigeria26–28 indicating a negative correlation between poor quality of life and negative emotions like anxiety and unhappiness. In response to individual questions, the majority of participants reported experiencing moderate pain, being content with their daily activities, feeling full and able to concentrate, and having negative thoughts. Around same mean score [55.17 ± 12.50 and 54.61 ± 11.92] were observed on other study conducted by Ganesh K et al.29 However, it was inconsistent with the study of Azar FEF et al.27 Also, moderate patients were satisfied with their sleep and work capacity. Higher mean score was observed on similar studied conducted by Fahad Saqib et al.30 Bhavit Oza et al. compared to a prior study from Brazil, the analyzed individual domain scores [55.55 ± 9.02 and 47.51± 9.06] were lower, which once more indicates that our research population has poorer QOL. This might be because the study sample had more co-morbid conditions and greater symptom scores. A small amount may also be caused by the population’s poor nutritional status as reported to general hospitals.19,31 Melchiors et al. analyzed and reported higher physical and psychological domain score 61.5 (95%CI from 59.0 to 64.1) and 65.7 (95%CI from 63.2 to 68.2).2,31
This study shows an improvement in HRQOL in a sample of people with hypertension who are representative. We looked at how QOL related to several sociodemographic, physical, environmental, and psychological variables. The use of the WHOQOL-BREF questionnaire to assess life quality was a strength of our study, which has established its acceptability, reliability, and validity. The study’s drawback, however, was the smaller sample size. The results cannot be generalized because of the limited sample size and the fact that the study only included patients with hypertension from one center. Larger sample size multi-centric research is therefore needed in this direction.
CONCLUSION
The improvement of HRQOL has become a top priority in health research as a result of physicians, scientists, and policymakers realizing the value of the patient’s self-rated experience beyond or in addition to objective and clinical measurements of health. According to the current study’s findings, the physical WHOQOL-BREF domain had a higher mean score than the psychological domain, indicating that negative feelings had a stronger detrimental effect on the health-related quality of life of hypertension patients. A higher quality of life was found to be positively correlated with male gender, older age (60-69 years), negative feelings, and lack of education, but not with female gender, older age (60-69 years), primary education, or negative feelings.
Cite this article
Shah SP, Borah GP, Bansal A, Bhatti K, Das R, Mehta DK. Impact of Anti-hypertensive Medication on Physical and Psychological Health Related Quality of Life (HRQOL) in Hypertensive Patients. J Young Pharm. 2023;15(2):372-9.
ACKNOWLEDGEMENT
The authors wish to thank Maharishi Markandeshwar (Deemed to be University), Mullana, India for all necessary facilities.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
References
- Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: A cross-sectional study in Urban Varanasi. Int J Hypertens. 2017;2017:5491838 [PubMed] | [CrossRef] | [Google Scholar]
- Adamu K, Feleke A, Muche A, Yasin T, Mekonen AM, Chane MG, et al. Health related quality of life among adult hypertensive patients on treatment in Dessie City, Northeast Ethiopia. PLOS ONE. 2022;17(9):e0268150 [PubMed] | [CrossRef] | [Google Scholar]
- Saini M, Rana M, Bhatti K, Das R, Kumar MD. Understanding health related quality of life in hypertensive patients: Interrogating effect of psychological and environmental factors. J Young Pharm. 2022;14(1):100-5. [CrossRef] | [Google Scholar]
- Jackson RE, Bellamy MC. Antihypertensive drugs. BJA Educ. 2015;15(6):280-5. [CrossRef] | [Google Scholar]
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J, et al. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365(9455):217-23. [PubMed] | [CrossRef] | [Google Scholar]
- Kaliyaperumal S, Hari S, Siddela P, Yadala S. Assessment of quality of life in hypertensive patients. J App Pharm Sci. 2016:143-7. [CrossRef] | [Google Scholar]
- Lenz TL, Monaghan MS. Lifestyle modifications for patients with hypertension. J Am Pharm Assoc (2003). 2008;48(4):e92-9. quiz e100 [PubMed] | [CrossRef] | [Google Scholar]
- Smith KW, Avis NE, Assmann SF. Distinguishing between quality of life and health status in quality of life research: A meta-analysis. Qual Life Res. 1999;8(5):447-59. [PubMed] | [CrossRef] | [Google Scholar]
- Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622-9. [PubMed] | [CrossRef] | [Google Scholar]
- Akonoghrere R, Aghoja O, Betiku O, Adje Z, Oparah A. An assessment of quality of life of hypertensive patients visiting a hospital in Warri, Nigeria. Acta Sci Pharm Sci. 2020;4(7):49-54. [PubMed] | [CrossRef] | [Google Scholar]
- DeJean D, Giacomini M, Vanstone M, Brundisini F. Patient experiences of depression and anxiety with chronic disease: A systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13(16):1-33. [PubMed] | [Google Scholar]
- Stein JD, Brown GC, Brown MM, Sharma S, Hollands H, Stein HD, et al. The quality of life of patients with hypertension. J Clin Hypertens (Greenwich Conn). 2002;4(3):181-8. [PubMed] | [CrossRef] | [Google Scholar]
- Bardage C, Isacson DG. Hypertension and health-related quality of life. An epidemiological study in Sweden. J Clin Epidemiol. 2001;54(2):172-81. [PubMed] | [CrossRef] | [Google Scholar]
- Klocek M, Kawecka-Jaszcz K. [Quality of life in patients with essential arterial hypertension. Part I: The effect o socio-demographic factors]. Przegl Lek. 2003;60(2):92-100. [PubMed] | [Google Scholar]
- World Health Organization. World Health Organization. 1996 [[cited Jan 15 2023]]. Available from: https://apps.who.int/iris/handle/10665/63529
Division of mental health. WHOQOL-bref: Introduction, administration, scoring and generic version of the assessment: Field trial version, December 1996 [Homepage on the Internet]. - Parkash J, Kalhan M, Singhania K, Punia A, Kumar B, Kaushal P, et al. Prevalence of hypertension and its determinants among policemen in a City of Haryana, India. Int J Appl Basic Med Res. 2019;9(3):143-7. [PubMed] | [CrossRef] | [Google Scholar]
- Narang S, Singh M, Yada J, Dixit S, Singh N. Prevalence of hypertension amongst employee’s state insurance beneficiaries of four districts in Haryana. Int J Community Med Public Health. 2020;7(2):604-8. [CrossRef] | [Google Scholar]
- WHOQOL. Measuring quality of life| The World Health Organization [Homepage on the Internet]. [[cited Jan 16 2023]]. Available from: https://www.who.int/tools/whoqol
- Oza BB, Patel BM, Malhotra SD, Patel VJ. Health related quality of life in hypertensive patients in a tertiary care teaching hospital. J Assoc Physicians India. 2014;62(10):22-9. [PubMed] | [Google Scholar]
- Xiao M, Zhang F, Xiao N, Bu X, Tang X, Long Q, et al. Health-related quality of life of hypertension patients: A population-based cross-sectional study in Chongqing, China. Int J Environ Res Public Health. 2019;16(13):23-48. [PubMed] | [CrossRef] | [Google Scholar]
- Youssef RM, Moubarak II, Kamel MI. Factors affecting the quality of life of hypertensive patients. East Mediterr Health J. 2005;11(1-2):109-18. [PubMed] | [Google Scholar]
- Wang C, Lang J, Xuan L, Li X, Zhang L. The effect of health literacy and self-management efficacy on the health-related quality of life of hypertensive patients in a western rural area of China: A cross-sectional study. Int J Equity Health. 2017;16(1):58 [PubMed] | [CrossRef] | [Google Scholar]
- Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. [Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref]. Rev Saude Publica. 2000;34(2):178-83. [PubMed] | [CrossRef] | [Google Scholar]
- Sprangers MA, Regt de EB, Andries F, Van Agt HM, Bijl RV, De Boer JB, et al. Which chronic conditions are associated with better or poorer quality of life?. J Clin Epidemiol. 2000;53(9):895-907. [PubMed] | [CrossRef] | [Google Scholar]
- Bulpitt CJ, Dollery CT, Carne S. Change in symptoms of hypertensive patients after referral to hospital clinic. Br Heart J. 1976;38(2):121-8. [PubMed] | [CrossRef] | [Google Scholar]
- Ha NT, Duy HT, Le NH, Khanal V, Moorin R. Quality of life among people living with hypertension in a rural Vietnam community. BMC Public Health. 2014;14(1):833 [PubMed] | [CrossRef] | [Google Scholar]
- Azar FEF, Solhi M, Chabaksvar F. Investigation of the quality of life of patients with hypertension in health centers. J Educ Health Promot. 2020;9(1):185 [PubMed] | [CrossRef] | [Google Scholar]
- Adedapo ADA, Akunne OO, Adedokun BO. Comparative assessment of determinants of health-related quality of life in hypertensive patients and normal population in south-west Nigeria. Int J Clin Pharmacol Ther. 2015;53(3):265-71. [PubMed] | [CrossRef] | [Google Scholar]
- Kumar SG, Majumdar A, G P. Quality of Life (QOL) and its associated factors using WHOQOL-bref among elderly in Urban Puducherry, India. J Clin Diagn Res. 2014;8(1):54-7. [PubMed] | [CrossRef] | [Google Scholar]
- Lodhi FS, Montazeri A, Nedjat S, Mahmoodi M, Farooq U, Yaseri M, et al. Assessing the quality of life among Pakistani general population and their associated factors by using the World Health Organization’s quality of life instrument (WHOQOL-bref): A population based cross-sectional study. Health Qual Life Outcomes. 2019;17(1):9 [PubMed] | [CrossRef] | [Google Scholar]
- Melchiors AC, Correr CJ, Pontarolo R, Santos Fde Ode S, Pe Souza RAde. Quality of life in hypertensive patients and concurrent validity of Minichal-Brazil. Arq Bras Cardiol. 2010;94:357-64. [PubMed] | [CrossRef] | [Google Scholar]
