ABSTRACT
Background:Parasitic infections have become a serious threat to the lives of human beings and animals and helminthiasis is the major parasitic infection. A wide range of anthelmintic agents have been used to treat these parasitic infections. Synthetic anthelmintic has various limitations like resistance. So, the major practical way of developing efficacious and cheaper anthelmintics is to consider herbal plants. Materials and Methods: The three plants selected in the study are Citrus medica, Coleusaromaticus and Murraya koenigii, belonging to the family Rutaceae, Lamiaceae and Rutaceae respectively. Traditionally, all these plants are used as vermicides. The main goal of the study was to examine the anthelmintic activity of these three plants using earthworms (Pheretima posthuma). 50% Hydroethanolic extracts of the three plants at different concentrations (20, 50, 80 mg/ml) showed dose-dependent anthelmintic response. Results: At concentrations of 20, 50, 80 mg/ml, all three plant extracts caused paralysis at 16.4, 28.33, 28.17, 11.35, 23.17, 22.4, 9.1, 19.33, 19.21 min. and death at 60.1, 84.56, 40.06, 46.08, 67.06, 37.42, 25.54, 56.56, 29.35 min. respectively. Albendazole was used as a reference standard at three different concentrations 20, 50, 80 mg/ml and caused paralysis at 40.37, 36.12, 24.44 min and death at 50.1, 39, 30.49 min. Conclusion: After analysing results, it was concluded that the three plants possess effective anthelmintic activity when compared with standard drug Albendazole and Citrus medica was found to be much more effective than all.
INTRODUCTION
Helminthiasis has been a major health issue in both humans and animals from ancient times. All kinds of helminth infections affect every second individual worldwide. Many efforts have been made to control parasitic infections with a level of utility and security over prototypes. Besides human complications, it also causes significant economic losses.1 Major causes of these infections are poor sanitation, malnutrition, lack of knowledge and practice about hygiene and an overcrowded population.2
The mode of transmission for helminthiasis is via humans and animals, acting as primary and secondary hosts. Insects act as the vector for the host, contaminating soil, water and food. It is a wide-spread, neglected tropical disease of developing countries and affects majorly poor people. Over 200 million people and 600 million school-year-aged children are diagnosed with parasites.3 The helminthic parasites weaken the immune system and increase susceptibility to HIV/AIDS, pneumonia, tuberculosis and malaria.4
Citrus medica(galgal, vetas)belongs to the family Rutaceae. It resembles a lemon but its size is larger than lemon, originate in the ignoble sections of Himalaya and after Gadwall to Sikkim, Assam and Ghats in the western direction. Leaves are beneficial in fatigue, asthma, cancer, diarrhoea, hyperthermia, halitosis, tumours, haemorrhoids, intestinal complaints, jaundice, skin diseases, and dysmenorrhoea and worm infections. Pharmacologically, it is analgesic, hypoglycaemic, antiulcer, anthelmintic, anticancer, hepatoprotective, estrogenic, hypolipidemic activity. Erucylamide and isolimonen are the important constituents in leaf with linalool, γ- terpinene, citral derivatives, isopulegol, cymene, geranial and α-terineol.5–15
Coleusaromaticus (Patta ajvaayana, Mexican mint) belongs to the family Lamiaceae. C. aromaticus is a green, persistent bush; leaves are aromatic like oregano cultivated throughout India, majorly found in Ceylon and Moluccas. Leaves Decoction governing severe cough, asthma, spasm. It is beneficial in epilepsy, nervous tension, rheumatism and dyspepsia. It is also used as a remedy for kidney stones, vaginal discharge, and dysfunction of the liver. Pharmacologically, it is antiepileptic, antitumor and nephron-protective. Mains of essential oil are carvacrol, thymol with rosmarinic acid, eugenol, chavicol, eucalyptol, pinene, caryophyllene, 1, 8-cineole, phellandrene.16–26
Murraya koenigii (Kari patta) belongs to the family Rutaceae. It is a defenceless shrub found in the Himalaya, Uttarakhand, Sikkim, Bengal, Garhwal, Western Ghats, Assam and Travancore-Cochin. Paste of leaves applied on bruises and eruptions cure itching and inflammation. This is also useful in poisonous animal bites, piles, leukoderma and other skin problems owing to its blood purifier activity. Pharmacologically, it is topoisomerase I and II inhibitor, antidiarrheal, mosquitocidal. Its main constituents present in roots are different types of alkaloids like mucoline, o-methyl murrayanine, 3-methyl carbazole, eustifolin-D, mahanine, mahanimbine, girinimbine, girinimbilol, mukoenin-A with essential oil like linalool, bornyl acetate, dehydro aromadendrene.27–37
MATERIALS AND METHODS
Plant Collection and Extraction
Leaves of Citrus medica, roots of Murraya koenigii and roots of Coleus aromaticus were collected from Malerkotla nursery, Punjab. Verification of all plant parts was done by NISCAIR, Delhi with authenticated numbers NISCAIR/RHMD/Consult/2019/3215-16-7, NISCAIR/RHMD/Consult/2019/3298-99-2, NISCAIR/RHMD/ Consult/2019/3215-16-5 for Citrus medica, Coleus aromaticus and Murraya koenigii respectively. Minimum 500g quantity of each plant part was shade dried, powdered and kept in contact with solvent in a stopper container for 3 days (maceration technique). The extract was concentrated by rotary vacuum evaporator and evaporation was done until it dried completely. The percentage yield of 50% hydroethanolic extract for each plant was calculated by the formula W1 (weight of residue after solvent evaporation) x100/ W2 (weight of powder taken initially).
Extracts of three plants were i.e Citrus medica blackish green with percentage yield 4.80, Coleus aromaticus golden brown with percentage yield 25, Murraya koenigii dark greenish with percentage yield 16.
Animals
Healthy adult Indian earthworms, zoologically, Pheretima posthuma (3 to 5-centimeter-long and 0.1 to 0.2 cm in diameter) were collected locally in the rainy season from June to September and were identified via Zoologist. Worms washed with normal saline solution (0.9 % w/v NaCl) and then used for study.38–39
Drugs and Chemicals
The drug albendazole (Standard anthelmintic) was procured from Apple Biotech Ludhiana, Punjab on a gratis basis along with complete analytical data. All solvents (organic) and chemicals of analytical grade are obtained from SD Fine Chemical Limited, Mumbai.
Determination of Anthelmintic Activity
The dried plant extracts were investigated for in vitro anthelmintic activity on earthworms as per method of Sravani and Paarakh,40
2011.Extracts were suspended in normal saline with Tween 80 (0.1 % v/v). Albendazole (5 mg/ml) was used as a standard drug. Observations were made in minutes by calculating the time taken to cause paralysis and death of the individual earthworm up to four hours of the test dated. Paralysis was supposed to occur once. The worm didn’t resuscitate even in 0.9 % w/v saline water. Death settles when a worm mislays its movement or integrity by vanishing away from its body colour. The consequences were recorded in terms of anthelmintic activity (minute) of each extractive. The anthelmintic activity of each plant 50 % hydroethanolic extract was evaluated on three changed attentions, 20, 50, 80 mg/ml as per the method of Sravani and Paarakh, 2011. All the dried plant extracts were suspended in normal saline Tween 80 (0.1% v/v) solution and properly labelled before starting the experiment. Total fourteen groups were made.
Group-1: (I control), Group-2: (vehicle) I ml of 0.1 percent v/v Tween 80 in 0.9 percent w/v NaCl, Group-3 Albendazole (20 mg/ml), Group-4: C. medica (20 mg/ml), Group-5: C. aromaticus (20 mg/ml), Group-6: M. koenigii (20 mg/ml), Group-7: Albendazole (50 mg/ml), Group-8: C. medica (50 mg/ml), Group-9: C. aromaticus (50 mg/ml), Group-10: M. koenigii (50 mg/ml), Group-11: Albendazole (80 mg/ml), Group-12: C. medica (80 mg/ml), Group-13: C. aromaticus (80 mg/ml), Group-14: M. koenigii (80 mg/ml).
Every time, a 20 ml volume of an extract solution was poured into petridish containing six healthy earthworms and repeated over three times (n=3) for each concentration. Three different concentrations 20, 50, 80 mg/ml, were prepared by dissolving 1.2 g, 3 g, 4.8 g in 60 ml of 0.9 percent w/v NaCl normal saline respectively. Each solution also contains 1 ml of Tween 80 (0.1% v/v). Remarks ended up to 4 hr because of the time taken for paralysis and death of worms in minutes.
RESULTS
The results of the anthelmintic activity of the above-mentioned plants at three different concentrations, i.e. 20, 50, 80 mg/ml respectively are summarized in Table 1. Remarks ended up to 4 hr for the time taken to paralysis and death of worms in minutes.
| Sl.no. | Group | Paralysis / Death | n1 | n2 | n3 | Mean | Sd | Sem | M ± Sem (n= 3) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | I | – | – | – | – | – | – | – | – |
| 2 | II | ||||||||
| 3 | III | Paralysis | 36.58 | 45.16 | 39.37 | 40.37 | 4.38 | 1.46 | 40.37 ±1.46 |
| Death | 46.12 | 54.59 | 49.59 | 50.10 | 4.26 | 1.42 | 50.10 ±1.42 | ||
| 4 | IV | Paralysis | 18.54 | 14.45 | 16.21 | 16.40 | 2.05 | 0.68 | 16.40 ±0.68 |
| Death | 64.43 | 56.39 | 59.48 | 60.10 | 4.06 | 1.35 | 60.10 ±1.35 | ||
| 5 | V | Paralysis | 25.19 | 31.33 | 28.47 | 28.33 | 3.07 | 1.02 | 28.33 ±1.02 |
| Death | 79.54 | 90.58 | 83.56 | 84.56 | 5.59 | 1.86 | 84.56 ±1.86 | ||
| 6 | VI | Paralysis | 27.53 | 30.57 | 26.41 | 28.17 | 2.15 | 0.72 | 28.17 ±0.72 |
| Death | 39.51 | 44.44 | 36.23 | 40.06 | 4.13 | 1.38 | 40.06 ±1.38 | ||
| 7 | VII | Paralysis | 35.11 | 36.09 | 37.16 | 36.12 | 1.03 | 0.34 | 36.12 ±0.34 |
| Death | 37.51 | 39.45 | 40.05 | 39.00 | 1.33 | 0.44 | 39± 0.44 | ||
| 8 | VIII | Paralysis | 10.35 | 11.55 | 12.15 | 11.35 | 0.92 | 0.31 | 11.35 ±0.31 |
| Death | 45.14 | 46.07 | 47.02 | 46.08 | 0.94 | 0.31 | 46.08 ±0.31 | ||
| 9 | IX | Paralysis | 25.38 | 20.58 | 23.56 | 23.17 | 2.42 | 0.81 | 23.17 ±0.81 |
| Death | 68.02 | 66.12 | 67.05 | 67.06 | 0.95 | 0.32 | 67.06 ±0.32 | ||
| 10 | X | Paralysis | 22.33 | 25.41 | 19.46 | 22.40 | 2.98 | 0.99 | 22.4 ±0.99 |
| Death | 38 | 39.11 | 35.14 | 37.42 | 2.05 | 0.68 | 37.42 ±0.68 | ||
| 11 | XI | Paralysis | 22.56 | 24.45 | 26.3 | 24.44 | 1.87 | 0.62 | 24.44 ± 0.62 |
| Death | 28.00 | 31.37 | 32.11 | 30.49 | 2.19 | 0.73 | 30.49 ±0.73 | ||
| 12 | XII | Paralysis | 9.02 | 9.14 | 9.14 | 9.10 | 0.07 | 0.02 | 9.1 ±0.02 |
| Death | 24.16 | 25.12 | 27.33 | 25.54 | 1.63 | 0.54 | 25.54 ±0.54 | ||
| 13 | XIII | Paralysis | 18.36 | 20.21 | 19.42 | 19.33 | 0.93 | 0.31 | 19.33 ±0.31 |
| Death | 58.26 | 56.16 | 55.25 | 56.56 | 1.54 | 0.51 | 56.56 ±0.51 | ||
| 14 | XIV | Paralysis | 18.05 | 20.06 | 19.53 | 19.21 | 1.04 | 0.35 | 19.21 ±0.35 |
| Death | 28.55 | 30.42 | 29.09 | 29.35 | 0.96 | 0.32 | 29.35 ±0.32 |
DISCUSSION
The problem of anthelmintic resistance, toxicity, and the increasing concern over the presence of drug deposits in animal products has led to a rebirth of curiosity in the use of plant based drugs.41 The use of natural dietary and herbal constituents has control of it which may decrease this dependence on drug treatment, and reduce the development of resistance.42 Plant materials estimated in the present-day study have been identified from several sources to serve as anthelmintic agents by traditional healers of Ethiopia. In vitro techniques are chosen over in vivomethods due to their low cost, simplicity, and rapid turnover.41
The present study involves a statistically significant relation between various graded concentrations of the extracts, the exposure test-time interval, and adult parasite mortality.43 The earthworms selected for the anthelmintic activity were the utmost sensitive to the 50% hydroethanolic extract of Citrus medica as can be seen in Figure 1. The graph defines the dose-dependent paralysis ranging from loss of movement to loss of response to external stimuli, which eventually proceeds to death. Our results define the importance of assessing anthelmintic compounds against not only free-living parasites but also parasitic stages. At 20, 50 and 80 mg/ml concentrations, Citrus medica extract caused paralysis at 16.40, 11.35, 9.1 min and death at 60.1, 46.08, 25.54 respectively. The hydroethanolic extracts of C. aromaticus and M. koenigii also exhibited dose dependent anthelmintic response that caused paralysis at 28.33, 28.17 min (20 mg/ml); 23.17, 22.4 min (50 mg/ml); 19.33, 19.21 min (80 mg/ml) and death at 84.56, 40.06 min (20 mg/ml); 67.06, 37.42 min (50 mg/ml); 56.56, 29.35 min (80 mg/ml) post treatment (Figure 1). All the hydroethanolic extracts of three plants were highly effective in causing the death of the worms as well as causing paralysis.
The anthelmintic activity of all the three plants may be due to the presence of polyphenolic compounds. The activity of Citrus medica to cause paralysis of worms in a short time suggests that it could be effective against parasitic infections of humans. These classes of plant secondary metabolites are considered to be the main sources of chemical constituents responsible for a large range of therapeutic activities of several medicinal plants. Some studies are available for anthelmintic activity of polyphenols, tannins, alkaloids, and flavonoids.44 The presence of these phytochemicals may be responsible for the observed anthelmintic activity of plant extracts in the present study.
Further studies are required to identify the actual constituents present in the extract which are responsible for activity against earthworms. It would be worthwhile to isolate pure compounds present in this plant responsible for activity as prototypes to synthesize their congeners, also to establish the effectiveness and pharmacological rationale for the use of Citrus medica as an anthelmintic drug.
CONCLUSION
It is concluded on the origin of the fallouts found by current study that floras can be considered as the substantial cause of accepted anthelmintic compounds in contradiction of digestive infections. The traditional use of these plants as folk remedies and putative anthelmintics by the people of India is also supported by the present study. All the plants showed concentration-dependent response against earthworm motility. Out of all the plants, Citrus medica was found to be highly active and potent to cause paralysis. The drug albendazole was used as a standard drug for comparison. But there’s a need to explore further this plant extract and precise mode of action in detail for delineation of their therapeutic efficacy, so that new drug molecules come into the market painstakingly as a principal of forthcoming that might avert helminthiasis and its associated health matters. It would be worthwhile to take pure compounds present in this plant as prototypes to synthesize their congeners that are edible for use in human and veterinary both. This will be a potent, effective and economical anthelmintic agent in future provided further studies are done focusing on the precise mechanism of action and in vivo study with other animal models.
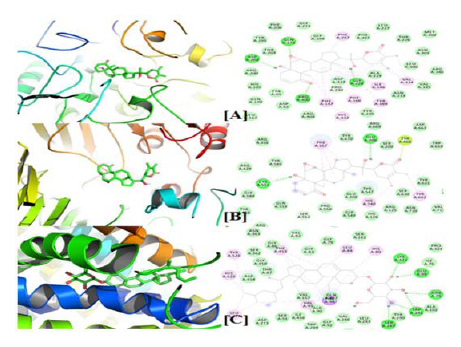
Figure 1.
Summarized paralysis and death time (in minute) at concentrations 20,50,80 mg/ml in Comparison to Albendazole (standard drug)
Cite this article
Singla S, Kaur S, Chopra A, Jindal A, Kaur D, Kaur N. In vitro Anthelmintic Activity of Three Vegetative Herbs. J Young Pharm. 2022;14(4):394-7.
ACKNOWLEDGEMENT
The authors are grateful to Prof. Satvinder Kaur, Principal, G.H.G. Khalsa College of Pharmacy, Gurusar Sadhar, Ludhiana, Punjab (India) for providing the facilities to do this work. The authors also wish to acknowledge the management and laboratory staff of the institute to carry out the research work and manpower. We acknowledge the NISCAIR for plant authentication and IKG PTU for providing a suitable environment.
References
- Idris OA, Wintola OA, Afolayan AJ. Helminthiases; prevalence, transmission, host-parasite interactions, resistance to common synthetic drugs and treatment. Heliyon. 2019;5(1) [PubMed] | [CrossRef] | [Google Scholar]
- Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J, et al. Helminth infections: The great neglected tropical diseases. J Clin Invest. 2008;118(4):1311-21. [PubMed] | [CrossRef] | [Google Scholar]
- Hotez PJ, Fenwick A, Savioli L, Molyneux DH. Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009;373(9674):1570-5. [PubMed] | [CrossRef] | [Google Scholar]
- Gloeckner C, Garner AL, Mersha F, Oksov Y, Tricoche N, Eubanks LM, et al. Repositioning of an existing drug for the neglected tropical disease onchocerciasis. Proc Natl Acad Sci U S A. 2010;107(8):3424-9. [PubMed] | [CrossRef] | [Google Scholar]
- Nicolosi E, Malfa SL, Mohamed EO, Negbi M, Goldscmidt EE. The search for the authentic citron: Historic and Genetic Analysis; Horticultural Science. Horticult Sci. 2005;40(7):1963-68. [PubMed] | [CrossRef] | [Google Scholar]
- Jitin R. An ethnobotanical study of medicinal plants in Taindol village, district Jhansi, Region Bundelkhand, Uttar Pradesh, India. J Med Plants Stud. 2013;1(5):59-71. [PubMed] | [CrossRef] | [Google Scholar]
- The ayurvedic pharmacopoeia of India, Part I. Vol. III. 2001:27-8. New Delhi: Government of India [PubMed] | [CrossRef] | [Google Scholar]
- Kirtikar KR, Basu BD, Singh BP, Singh MP. Indian medicinal plants Dehradun. 1993:485-90. [PubMed] | [CrossRef] | [Google Scholar]
- Arias BA, Ramón-Laca L. Pharmacological properties of citrus and their ancient and medieval uses in the Mediterranean region. J Ethnopharmacol. 2005;97(1):89-95. [PubMed] | [CrossRef] | [Google Scholar]
- Ajaiyeoba EO, Oladepo O, Fawole OI, Bolaji OM, Akinboye DO, Ogundahunsi OA, et al. Cultural categorization of febrile illnesses in correlation with herbal remedies used for treatment in Southwestern Nigeria. J Ethnopharmacol. 2003;85(2-3):179-85. [PubMed] | [CrossRef] | [Google Scholar]
- Sivakumar N, Venkataraman R. Phytochemical and pharmacological studies on plant waste materials. Pharm Sin. 2010;1(1):1-6. [PubMed] | [CrossRef] | [Google Scholar]
- Bhuiyan MN, Begum J, Sardar PK, Rahman MS. Constituents of peel and leaf essential oils of Citrus medica L. J Sci Res. 2009;1(2):387-92. [CrossRef] | [Google Scholar]
- Albach RF, Redman GH. Composition and inheritance of flavanones in Citrus fruit. Phytochemistry. 1969;8(1):127-43. [CrossRef] | [Google Scholar]
- Andrews AC. Acclimatization of citrus fruits in the Mediterranean Region. Agricul Hist. 1961;35(1):35-46. [CrossRef] | [Google Scholar]
- Mizuno M, Ohara M, Syumiya K, Matsuo S, Linuma M, Tanaka T, et al. Chemotaxonomic studies on the genus Citrus: III. Coumarins in Citrus intermedia and Citrus medica Yakugaku Zasshi. 1989;43:259-61. [CrossRef] | [Google Scholar]
- Harborne JB, Warrier PK, Nambiar VP. Indian Medicinal Plants: A Compendium of 500 Species. 1995;4(1):315-17. [CrossRef] | [Google Scholar]
- Faleiro L, Miguel G, Gomes S, Costa L, Venâncio F, Teixeira A, et al. Antibacterial and antioxidant activities of essential oils isolated from L (Cav.) and L. J Agric Food Chem. 2005;53(21):8162-8. [PubMed] | [CrossRef] | [Google Scholar]
- Dragland S, Senoo H, Wake K, Holte K, Blomhoff R. Several culinary and medicinal herbs are important sources of dietary antioxidants. J Nutr. 2003;133(5):1286-90. [PubMed] | [CrossRef] | [Google Scholar]
- Chatterjee A, Pakrashi SC. Plants used in the Ayurvedic system in Indian medicine and also in modern medicine. The Treatise on Indian Medicinal Plants. 1997:8-13. New Delhi: National Institute of Science Communication [PubMed] | [CrossRef] | [Google Scholar]
- Dutta S. Essential oil of of Indian origin. Indian Oeil Soap J. 1959;25:120 [PubMed] | [CrossRef] | [Google Scholar]
- Knab MK, Heather E, Marta K. Isolation of the compounds in Mentha piperita, Mentha spicata and . Abstracts of the papers 238th ACS national meeting; Aug 16-20 2009; Washington, DC, United States. [PubMed] | [CrossRef] | [Google Scholar]
- Sahaykhare R, Banerjee S, Kundu K. Array. Int J Pharm Biol Sci. 2011;2(3):488-500. [PubMed] | [CrossRef] | [Google Scholar]
- Weehuizen F. The phenol from the leaves of Lour. Recl Trav Chim Pays-Bas. 1918;37:355-56. [PubMed] | [CrossRef] | [Google Scholar]
- Nick A, Rali T, Sticher O. Biological screening of traditional medicinal plants from Papua New Guinea. J Ethnopharmacol. 1995;49(3):147-56. [PubMed] | [CrossRef] | [Google Scholar]
- Wadikar DD, Patki PE. Array. J Food Sci Technol. 2016;53(7):2895-901. [PubMed] | [CrossRef] | [Google Scholar]
- Rout OP, Acharya R, Mishra SK, Sahoo R. Pathorchur (): A review of the medicinal evidence for its phytochemistry and pharmacology properties. Int J Applied Biology and Pharm Tech. 2012;3(4):348-55. [PubMed] | [CrossRef] | [Google Scholar]
- Jain M, Gilhotra R, Singh RP, Mittal J, Leaf C. (): A spice with medicinal property. Moj Biol Med. 2017;2(3):236-57. [PubMed] | [CrossRef] | [Google Scholar]
- Gupta P, Nahata A, Dixit VK. An update on spreng: A multifunctional Ayurvedic herb. Zhong Xi Yi Jie He Xue Bao. 2011;9(8):824-33. [PubMed] | [CrossRef] | [Google Scholar]
- Raghunathan K, Mitra R. Pharmacognosy of indigenous drugs, central council for research in Ayurveda and Siddha, New Delhi. 1982:433 [PubMed] | [CrossRef] | [Google Scholar]
- Handrail H, Pandith A, Shruthi SD. A review on : Multipotential medicinal plant. Asian J Pharm Clin Res. 2012;5(4):05-14. [PubMed] | [CrossRef] | [Google Scholar]
- Kumar VS, Sharma A, Tiwari R, Kumar S. Array. J Med. Arom. Plant Sci. 1999;21(4):1139-44. [PubMed] | [CrossRef] | [Google Scholar]
- Srivastava SK, Srivastava SD. New constituents and biological activity of the roots of . J Indian Chem Soc. 1993;70(7):655-9. [PubMed] | [CrossRef] | [Google Scholar]
- Ito C, Thoyama Y, Omura M, Kajiura I, Furukawa H. Alkaloidal Constituents of . Isolation and Structural Elucidation of Novel Binary Carbazolequinones and Carbazole Alkaloids. Chem Pharm Bull. 1993;41(12):2096-100. [CrossRef] | [Google Scholar]
- Kong YC, Ng KH, But PP, Li Q, Yu SX, Zhang HT, et al. Sources of the anti-implantation alkaloid yuehchukene in the genus . J Ethnopharmacol. 1986;15(2):195-200. [PubMed] | [CrossRef] | [Google Scholar]
- Joshi BS, Kamat VN, Gawad DH. On the structures of girinimbine, mahanimbine, Isomahanimbine, koenimbidine and murrayacine. Tetrahedron. 1970;26(6):1475-82. [PubMed] | [CrossRef] | [Google Scholar]
- Xie JT, Chang WT, Wang CZ, Mehendale SR, Li J, Ambihaipahar R, et al. Curry leaf ( Spreng) reduces blood cholesterol and glucose levels in ob/ob mice. Am J Chin Med. 2006;34(2):279-84. [PubMed] | [CrossRef] | [Google Scholar]
- Thorn GW, Adams RD, Brundwal E, Isselbacher KJ, Petersdort RG. Principles of internal medicines. 1977:1088-9. [PubMed] | [CrossRef] | [Google Scholar]
- Vigar Z. Atlas of medical parasitology RW. 1984:216-7. [PubMed] | [CrossRef] | [Google Scholar]
- Sravani T, Paarakh MP. Evaluation of anthelmintic activity of rhizomes of Buch. Ham Int J Res Pharm Sci. 2011;2(1):66-8. [PubMed] | [CrossRef] | [Google Scholar]
- Selamawit Z, Teka F, Solomon A. Array. Bio Med Res Int. 2017:1-6. [PubMed] | [CrossRef] | [Google Scholar]
- Andrew RW, Honorata MR, Christos F, Olivier D, Irene MH, Stig MT, et al. Assessment of the anthelmintic activity of medicinal plant extracts and purified condensed tannins against free-living and parasitic stages of Oesophagostomum dentatum. Parat Vec. 2014;518(7):1-12. [PubMed] | [CrossRef] | [Google Scholar]
- Aliyi HA, Mebrat E, Teka F, Dereje R, Bahar M, Solomon AH, et al. Array. J Parasitol Res. 2020;27:1-7. [PubMed] | [CrossRef] | [Google Scholar]
- Spiridoula A, Marit A, Jarkko H, Eva M, Nebojsa S, Havard S, et al. Chemical analysis and anthelmintic activity against [] of Nordic Bark Extracts . Front Vet Sci. 2021;8:1-9. [PubMed] | [CrossRef] | [Google Scholar]
