ABSTRACT
Backgroud
Blood Pressure (BP) variability is a crucial yet often overlooked factor in cardiovascular health, reflecting the dynamic nature of cardiovascular regulation in response to various stimuli. Among the factors influencing BP variability, body posture is particularly significant, as it can affect hemodynamics and blood flow. Furthermore, the Body Mass Index (BMI) serves as a critical indicator of body composition and health risk. Research has indicated that BMI can influence BP, but its interaction with postural changes remains less explored. Hence, the current study aimed to assess the BP variability in different sitting postures in correlation with BMI.
Materials and Methods
A cross-sectional descriptive study was carried out with the sample of 50 participants aged between 20 to 33 years. BP was measured according to the standardized protocol with mercury sphygmomanometer including four different sitting measurements: sitting with back rest and without crossed legs, sitting without back rest and without crossed legs, sitting with crossed legs and back rest, sitting with crossed legs and without back rest. BMI was calculated by dividing weight in kilograms by height in meters squared. Paired t-test and Pearson correlation were used for statistical analysis.
Results
Sitting with back rest without crossed legs showed significantly lower BP compared to other sitting postures. BP taken at the different sitting positions were positively related to each other with moderate to strong association. BMI was positively related to BP taken at sitting with crossed legs without back rest.
Conclusion
The findings of the study are expected to enhance the understanding of postural influences on cardiovascular health and contribute to more personalized recommendations for BP measurements at clinical set-up.
INTRODUCTION
Hypertension is a prevalent global health issue that necessitates accurate Blood Pressure (BP) measurement for effective diagnosis and management. Recent studies underscore the significant impact of body posture on BP readings, which is often overlooked in clinical practice. BP varies significantly with posture, notably decreasing when transitioning from supine to standing positions (Hossain et al., 2019). This highlights the need for consistent measurement protocols to prevent misdiagnosis or inappropriate treatment adjustments. Moreover, body composition plays a crucial role in BP variability. Higher Body Mass Index (BMI) and Waist Circumference (WC) are associated with greater increases in systolic BP upon standing, suggesting that adiposity significantly affects BP regulation during postural changes (Moreno Velasquez et al., 2022). These findings emphasize the importance of considering body composition in cardiovascular risk assessments. BMI and Waist-to-Height Ratio (WHT2R) have been identified as useful predictors for high BP and wide Pulse Pressure (PP), highlighting their relevance in clinical evaluations (Kang, 2021).
Additionally, prolonged sedentary behaviour, such as sitting, has been shown to adversely affect cardiovascular health. Increases in BP during prolonged sitting indicate potential risks associated with sedentary lifestyles (Alansareet al., 2020). Variability in central BP responses to upright posture identifies systemic vascular resistance and cardiac output as key factors influencing these changes. This suggests that traditional brachial BP measurements may not fully capture cardiovascular risk, underscoring the need to consider central hemodynamic.
Regular activity breaks during periods of prolonged sitting have been found to significantly improve vascular function compared to continuous sitting or standing. This highlights the potential risks associated with sedentary lifestyles and underscores the importance of incorporating movement into daily routines to mitigate cardiovascular risks (Peddieet al., 2021). Furthermore, different body postures can significantly influence cardiovascular responses. For instance, the right lateral recumbent position has been associated with the lowest blood pressure readings, while the bent position tends to record the highest. These findings suggest that posture plays a crucial role in BP variability, which is essential for understanding individual differences in cardiovascular measurements.
Collectively, these studies emphasize the complexity of BP regulation and its sensitivity to factors such as posture, body composition, and lifestyle behaviours. Understanding these dynamics is vital for improving hypertension diagnosis and management strategies, enabling healthcare providers to offer more personalized and effective interventions.
MATERIALS AND METHODS
The study aimed to investigate the effects of various sitting postures on BP measurements and their correlation with BMI. A total of 50 participants, aged between 20 and 33 years, were recruited. Participants provided informed consent before participating in the study. Demographic details such as name, age, gender, family history of hypertension and diabetes was recorded.
Inclusion criteria
- Both male and female participants.
- Participants willing to provide informed written consent.
- Participants must be able to maintain various sitting postures comfortably for the necessary duration.
- Participants free from diagnosed cardiovascular diseases, hypertension, or metabolic disorders.
Exclusion criteria
- Participants who smoke and have history of excessive alcohol intake.
- Participants taking antihypertensive, cardiovascular, or weight-modifying medications.
BP Measurement
BP was measured using a mercury sphygmomanometer, adhering to standardized guidelines to ensure consistency and reliability. Four different sitting postures were tested to observe variations in BP:
Sitting with a backrest and uncrossed legs.
Sitting without backrest and uncrossed legs.
Sitting with a backrest and crossed legs.
Sitting without backrest and crossed legs.
For each posture, the cuff was appropriately positioned on the participant’s upper arm, ensuring proper fit and placement at heart level. BP readings were recorded in the same environment to minimize external influences, with a rest period of at least 5 minutes between postures.
BMI Measurement
BMI was calculated for each participant to assess its potential correlation with BP readings. Height (in meters) was measured using a stadiometer, and weight (in kilograms) was measured using a calibrated digital scale. BMI was derived using the formula:
BMI=Weight (kg)/Height (m2)
STATISTICAL ANALYSIS
Data was analyzed using the following statistical methods
- Paired t-test: Used to compare BP measurements between the four sitting postures within the same individual, assessing statistically significant differences.
- Pearson correlation coefficient: Employed to examine the relationship between BMI and BP readings across different postures.
All analyses were performed using a statistical software package, with a significance level set at p<0.05. Results were presented as mean±Standard Deviation (SD) for BP readings and BMI. This approach allowed for a comprehensive evaluation of how sitting posture and BMI influence BP measurements.
RESULTS
A total of 50 students were involved in the study and 78% of the participants were females whereas 22% were males (Table 1). The average age of the participant was 22.68 years with a SD of 3.5 years. Among the respondents, 32% of them had a family history of hypertension and 30% of them had a family history of diabetes mellitus. More than half of students had normal weight (60%), 4% were underweight, 28% were overweight and 8% were obese (Table 1).
| Variable | |
| Age in years; mean (SD) | 22.68 (3.45) |
| Gender, n (%) | |
| Male | 11 (22) |
| Female | 39 (78) |
| Family history of hypertension, n (%) | |
| No | 34 (68) |
| Yes | 16 (32) |
| Family history of Diabetes, n (%) | |
| No | 35 (70) |
| Yes | 15 (30) |
| BMI, n (%) | |
| Underweight | 2 (4) |
| Normal weight | 30 (60) |
| Overweight | 14 (28) |
| Obese | 4 (8) |
Comparison of Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) in different sitting postures were displayed in Figures 1 and 2. Among different sitting postures, the median value of BP was highest in sitting without back rest and without crossed legs. The BP was noticed lowest at sitting with back rest and without crossed legs.
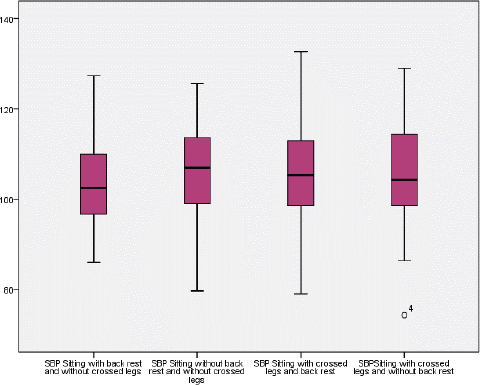
Figure 1:
Comparison of SBP in different sitting postures.

Figure 2:
Comparison of DBP in different sitting postures.
A paired t-test was performed to determine the differences between various sitting postures. Significant different results were noticed in three different pairs: pairs 1, 2 and 3. Sitting with back rest without crossed legs showed lower blood pressure compared to other postures (Table 2).
| Variable | Pairwise comparison | Mean difference | SD | p-value |
|---|---|---|---|---|
| SBP | 1. Back rest without crossed legs-without back rest without crossed legs. | -2.127 | 6.065 | 0.017* |
| 2. Back rest without crossed legs-back rest crossed legs. | -2.267 | 7.605 | 0.040* | |
| 3. Back rest without crossed legs-crossed legs without back rest. | -2.147 | 7.209 | 0.040* | |
| 4. Without back rest without crossed legs-back rest crossed legs. | -0.14 | 6.756 | 0.884 | |
| 5. Without back rest without crossed legs-crossed legs without back rest. | -0.02 | 8.969 | 0.987 | |
| 6. Back rest crossed legs -crossed legs without back rest. | 0.120 | 8.07 | 0.917 | |
| DBP | 1. Back rest without crossed legs-without back rest without crossed legs. | -2.633 | 5.588 | 0.002* |
| 2. Back rest without crossed legs-back rest crossed legs. | -2.040 | 6.26 | 0.025* | |
| 3. Back rest without crossed legs-crossed legs without back rest. | -2.453 | 6.162 | 0.007* | |
| 4. Without back rest without crossed legs-back rest crossed legs. | 0.593 | 5.764 | 0.470 | |
| 5. Without back rest without crossed legs-crossed legs without back rest. | 0.18 | 8.434 | 0.881 | |
| 6. Back rest crossed legs -crossed legs without back rest. | -0.413 | 8.186 | 0.723 |
A Pearson correlation test was carried out as shown in Tables 3 and 4 and the results showed that BMI is positively related to SBP taken at back rest without crossed legs and crossed legs without back rest. Regarding DBP, BMI was positively related to sitting with crossed legs without back rest. The strength of association between BP and sitting postures was weak. BP taken at the different sitting positions were positively related to each other with moderate to strong association.
| Measure | Mean | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Back rest and without crossed legs | 103.82 | 9.66 | 1 | |||
| 2. Without Back rest and without crossed legs | 105.95 | 10.43 | 0.820** | 1 | ||
| 3. Crossed legs and back rest | 106.09 | 10.54 | 0.720** | 0.792** | 1 | |
| 4. Crossed legs and without back rest | 105.97 | 11.47 | 0.780** | 0.668** | 0.734** | 1 |
| 5. BMI | 22.27 | 4.20 | 0.329* | 0.262 | 0.258 | 0.377** |
| Measure | Mean | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Back rest and without crossed legs | 65.20 | 8.19 | 1 | |||
| 2. Without back rest and without crossed legs | 67.83 | 9.92 | 0.826** | 1 | ||
| 3. Crossed legs and back rest | 67.24 | 9.41 | 0.755** | 0.823** | 1 | |
| 4. Crossed legs and without back rest | 67.65 | 7.81 | 0.704** | 0.569** | 0.561** | 1 |
| 5. BMI | 22.27 | 4.20 | 0.267 | 0.033 | 0.156 | 0.345* |
DISCUSSION
This study investigates the complex interactions between body posture, body composition, and BP variability. The findings align with existing literature, emphasizing the multifaceted nature of BP regulation and its implications for clinical practice.
Impact of Body Posture on BP
Body posture significantly influences BP measurements, with notable physiological mechanisms, such as changes in venous return and cardiac output, playing a role. Research has demonstrated marked reductions in both SBP and DBP when transitioning from supine to standing (Hossain et al., 2019), underscoring the importance of standardizing BP measurement protocols. Similarly, elevated BP levels in unsupported sitting positions are reported due to increased muscular strain (Severinet al., 2020). This aligns with our findings, which showed lower BP values in postures with back support, highlighting the necessity of incorporating back support into clinical BP measurement protocols. Our study complements findings from Quarteyet al. (2023), who observed varying BP levels across postural changes, suggesting posture-induced variability as a key factor in understanding individual differences in cardiovascular responses. Additionally, significant hemodynamic changes observed in children and adolescents when moving from supine to sitting without back support highlight the importance of posture in managing sitting intolerance symptoms (Taoet al., 2020). By integrating these observations, our study underscores the importance of postural considerations for accurate BP assessments.
Role of Body Composition
Our study corroborates the significant association between BMI and BP levels, as highlighted by previous research (Papathanasiouet al., 2015). Higher BMI is consistently linked to increased hypertension risk, reinforcing the need to consider body composition in cardiovascular risk assessments. Further studies emphasize that both BMI and WC are associated with postural increases in SBP, although BMI remains the dominant predictor (Moreno Velasquez et al., 2022). Kang (2021) explored associations between obesity indices like BMI and WHT2R with BP among Korean adults, finding both indices useful predictors for high BP and wide Pulse Pressure (PP). Similarly, visceral fat and Waist-Hip Ratio (WHR) have been identified as significant predictors of SBP among medical students, suggesting that central obesity measures may provide better insights into hypertension risks compared to general adiposity measures (Gandhiet al., 2020).
Mechanisms of Blood Pressure Regulation
The mathematical model developed by Olufsenet al. (2005) provides a comprehensive framework for understanding the physiological processes involved in BP regulation during postural changes. The model highlights the roles of autonomic regulation and cerebral autoregulation in maintaining cerebral perfusion despite gravitational challenges. This mechanistic insight is crucial for developing targeted interventions to manage orthostatic intolerance and related disorders. While smoking and physical activity levels were not significantly associated with BP in some studies, these lifestyle factors remain important considerations for overall cardiovascular health (Papathanasiouet al., 2015). Regular activity breaks during prolonged sitting significantly improve vascular function and reduce postprandial insulin levels compared to continuous sitting or standing, emphasizing the benefits of incorporating movement into daily routines (Peddieet al., 2021).
Clinical Implications
The findings from these studies highlight the necessity for healthcare providers to standardize BP measurement protocols that account for posture-related variability. This approach will enhance the accuracy of hypertension diagnosis and management strategies, ultimately improving patient outcomes. Additionally, ensuring back support during BP measurements can provide more consistent readings by reducing muscular strain and associated hemodynamic changes.
Limitations and Future Directions
While our study provides valuable insights into BP variability, it is essential to acknowledge limitations such as sample size and demographic diversity. Future research should explore these relationships in larger, more diverse populations to validate our findings further. Additionally, investigating genetic factors and their interaction with environmental influences could offer deeper understanding into BP regulation mechanisms.
CONCLUSION
This study underscores the significant role of sitting posture in influencing BP variability and highlights the need to consider posture and BMI in clinical BP measurements. Specifically, sitting with a backrest and without crossed legs was associated with lower BP readings, whereas individuals with higher BMI demonstrated greater variability in BP depending on their posture. These insights support the development of more precise and individualized BP measurement protocols, ultimately enhancing cardiovascular risk assessments and management strategies. Future research should validate these findings in larger, more diverse populations to strengthen the generalizability of the results. Investigating additional factors such as age, gender, and physical activity levels could provide a more comprehensive understanding of BP variability. Moreover, exploring the physiological mechanisms underlying these associations will be crucial in advancing hypertension diagnosis and treatment.
Cite this article:
George SD, Shuen FTY, Kumari U, Maung TM. Blood Pressure Variability in Different Siting Postures in Correlation with Body Mass Index. J Young Pharm. 2025;17(2):400-5.
ABBREVIATIONS
| BP | Blood Pressure |
|---|---|
| BMI | Body Mass Index |
| WC | Waist Circumference |
| WHT2R | Waist-to-Height Ratio |
| PP | Pulse Pressure |
| SD | Standard Deviation |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| WHR | Waist-Hip Ratio |
References
- Alansare AB, Kowalsky RJ, Jones MA, Perdomo SJ, Stoner L, Gibbs BB, et al. (2020) The effects of a simulated workday of prolonged sitting on seated versus supine blood pressure and pulse wave velocity in adults with overweight/obesity and elevated blood pressure. Journal of Vascular Research 57: 355-366 https://doi.org/10.1159/000510294 | Google Scholar
- Gandhi S, Sorout J, Raina R, Raina A, Miglani U, Manchanda K, Reddy S, et al. (2020) Association between blood pressure and obesity indices in medical students. Journal of Clinical and Diagnostic Research 14 https://doi.org/10.7860/JCDR/2020/44904.13953 | Google Scholar
- Islam MN, Kamal S, Islam MS, Hossain SA. (2019) Variation of blood pressure during change of posture. Bangladesh Medical Journal Khulna 51: 16-20 https://doi.org/10.3329/bmjk.v51i1-2.40461 | Google Scholar
- Kang NL. (2021) Association between obesity and blood pressure in common Korean people. Vascular Health and Risk Management 17: 371-377 https://doi.org/10.2147/VHRM.S316108 | Google Scholar
- Moreno Velásquez I, Jaeschke L, Steinbrecher A, Boeing H, Keil T, Janke J, Pischon T, et al. (2022) Association of general and abdominal adiposity with postural changes in systolic blood pressure: Results from the NAKO pretest and MetScan studies. Hypertension Research 45: 1964-1976 https://doi.org/10.1038/ s41440-022-01029-5 | Google Scholar
- Olufsen MS, Ottesen JT, Tran HT, Ellwein LM, Lipsitz LA, Novak V, et al. (2005) Blood pressure and blood flow variation during postural change from sitting to standing: Model development and validation. Journal of Applied Physiology 99: 1523-1537 https://doi.org/10.1152/japplphysiol.00177.2005 | Google Scholar
- Papathanasiou G, Zerva E, Zacharis I, Papandreou M, Papageorgiou E, Tzima C, Georgakopoulos D, Evangelou A, et al. (2015) Association of high blood pressure with body mass index, smoking and physical activity in healthy young adults. The Open Cardiovascular Medicine Journal 9: 5-17 https://doi.org/10.2174/1874192401509010005 | Google Scholar
- Peddie MC, Kessell C, Bergen T, Gibbons TD, Campbell HA, Cotter JD, Rehrer NJ, Thomas KN, et al. (2021) The effects of prolonged sitting, prolonged standing, and activity breaks on vascular function, and postprandial glucose and insulin responses: A randomised crossover trial. PLOS One 16 https://doi.org/10.1371/journal.pone.0244841 | Google Scholar
- Quartey P, Halm E, Yeboah-Arhin O. (2023) Postural changes in blood pressure and heart rate among healthy young adults in a Ghanaian university. International Journal of Current Research in Physiology and Pharmacology : 1-9 https://doi.org/10.1371/journal.pone.0244841 | Google Scholar
- Severin R, Sabbahi A, Albarrati A, Phillips SA, Arena S. (2020) Blood pressure screening by outpatient physical therapists: A call to action and clinical recommendations. Physical Therapy 100: 1008-1019 https://doi.org/10.1093/pt j/pzaa034 | Google Scholar
- Suojanen LJ, Koskela JK, Wilenius M, Choudhary MK, Hautaniemi EJ, Viik J, Mustonen JT, Pörsti IH, et al. (2021) Individual changes of central blood pressure in response to upright posture: Different hemodynamic phenotypes. Journal of Hypertension 39: 2403-2412 https://doi.org/10.1097/HJH.0000000000002965 | Google Scholar
- Tao C, Han Z, Yan Y, Pan Z, Zhu H, Li X, Li H, Wang Y, Liu P, Wang Y, Jiang M, Tang C, Jin H, Du J, et al. (2020) Sitting-induced hemodynamic changes and association with sitting intolerance in children and adolescents: A cross-sectional study. Scientific Reports 10 https://doi.org/10.1038/s41598-020-70925-y | Google Scholar
