ABSTRACT
Background: BBBBThe COVID-19 pandemic have led to both physical and psychological outbreaks in lives of many people, especially among quarantined people. To handle this mood disorders of isolated COVID-19 patient’s in home care, noninvasive OM chanting has been adopted to study its effect on stress, anxiety, depression, quality of sleep and life. Materials and Methods: 56 participants with the mean age of 41 years confirmed with COVID-19 infection under the Saveetha home care program were selected. The Experimental group practiced OM chanting for 20mins for a duration of 14 days. DASS-21 and Pittsburgh Sleep Quality Index was assessed before and after the intervention. Results: After 14 days’ intervention, significant decrease in depression (13.26±4.52 to 7.84±3.96; p=0.01), anxiety (14.38±5.28 to 8.29±4.73; p=0.05) and stress (16.88±4.90 to 7.32±3.91; p=0.05) were noted. In addition to that over all sleep quality (11.24± 3.89 to 6.70± 3.51) and quality of life also improved among the patients after the 14 days OM chanting. Conclusion: The practice of OM chanting for two weeks showed notable reduction in the DASS-21 in comparison to the first base assessment. The increase in the Pittsburgh Sleep Quality Index was also recorded. In further, larger sample size and long-term intervention will be studied with a robust research design.
INTRODUCTION
The outbreak of COVID-19 throughout the world was caused by the coronavirus SARS-CoV-2. Which was initially reported in China. The infected people developed fever, cold, tiredness, loss of smell, taste, breathlessness and many other less common symptoms.1 Not only physical symptoms but also mental symptoms were reported in COVID-19 patients like stress, depression and anxiety due to the quarantine.2 It also affects the immune system there by affecting the overall the quality of life.3 Though various drug management has been undertaken for the treatment of COVID-19, the practice of noninvasive traditional procedures like yoga and meditation have been proven effective in resolving psychological illness4 and has profound effects in reducing the inflammatory markers.5 The ancient technique like “Taoist yoga” “Vedic chanting” describes the power of sounds that is “Mantras”, which is known to alleviate depression, stress, and other mental disturbances by controlling the mind and body.6 In comparison to the normal ssss chanting, OM chanting induces deactivation of brain areas which are usually activated during stress and depression there by reducing the stress anxiety and depression levels.7 Overall, the impact of OM chanting on reducing stress, anxiety, and depression has been well recorded. Therefore, this can be adopted as a simple noninvasive technique to alleviate the psychological disturbances in COVID-19 patients with mild asymptomatic complaints.
MATERIALS AND METHODS
Study Participants
The willing COVID-19 patients with mild severity, who visited Saveetha home care program of Saveetha medical college and hospital, were screened by the medical staff of the Saveetha home care program and were included into the study who satisfied the inclusion and exclusion criteria.
Inclusion and Exclusion Criteria
Asymptomatic COVID-19 patients with mild severity, and under home isolation of both sex and adult patient ≥18 years and ≤60 years of age were included into the study.
Pregnant women, symptomatic patients like moderate or severe with other comorbidity conditions were excluded from the study.
We have selected 25 patients (15 males and 10 female) with the age range of 41 to 60-years.
Ethical Clearance
The study got approved by the Institute of Ethical Committee (SMC/ IEC/2020/08/038) of Saveetha Medical College and Hospital. From the participants informed consent form was obtained after explaining the full protocol in their convenient language.
Procedure
This is a quasi-experimental study conducted to assess the stress, depression, anxiety and sleep quality in home quarantined COVID-19 patients. All the recruited participant undergone 20 mins of intervention twice a day morning and evening for 14 days. Assessments were done before and immediately after interventions.
Assessments
The values of depression, anxiety, stress and sleep quality were assessed using theDASS-21 and Pittsburgh Sleep Quality Index (PSQI) questionnaires. The parameters were assessed before and after the AUM intervention through online platform.
DASS-21: for Assessing Depression, Anxiety and Stress
It assesses the depression, anxiety and stress of an individual using 7 items under each component. The cut-off scores of each component defines its range of severity from mild to extreme severe.8
Pittsburgh Sleep Quality Index (PSQI): For assessing sleep quality
It is a 19 self – rated questions, which are clubbed to form seven “component’ to assess the sleep quality. Higher the scores indicate the poor quality of sleep.9
WHOQOL-BREF
It consists of 26 questions to assess the overall perception of life quality and their health using the two main items. The four domains represent the physical health, psycological, social relationship and environment status of the individual. Higher the score better the quality of life.10
Intervention
The Continuous AUM chanting was done for 20 mins along the online platform, twice a day between 6.00-8.00am in the morning and between
4.00-6.00pm in the evening on empty stomach for 14 days (10).
Data analysis
R statistical software (Version 4.0.2) was used for the statistical analysis and a value with p<0.05 was considered statistically significant. Paired t-test was used to assess the overall effect of AUM chanting on the outcome variables.
RESULTS
Of the 88 patients contacted, 56 were enrolled and 32 did not comply with the eligibility criteria or not willing to participate in the study. None of the patients reported any adverse effects during the study. Demographical characteristics were presented in the Table 1.
| Characteristic | N(%)/Mean ± SD |
|---|---|
| Age | 48.52±9.78 |
| Gender (M/F) | 34/22 |
| Marital status (Yes/No) | 37/19 |
| Education Level | |
| Degree or above | 29(51) |
| School | 24(42.8) |
| Illiterate | 3(5.3) |
| Clinical symptoms | |
| Fever | 18(32) |
| Cough | 12(21) |
| Myalgia | 18(32) |
| Sore throat | 8 (14) |
After 14 days of OM chanting, the participants showed significant improvements in the psychological level, sleep quality and quality of life. Lower levels of depression (p=0.01), anxiety (p=0.05) and stress (p=0.05) was reported by analyzing through DASS-21, sleep quality (p=0.03) assessed through PSQI and quality of life improvements in general health (p=0.01), psychological (p=0.04), physical (p=0.01), social (p=0.02), and environmental wellbeing (p=0.01) of quality of life measured by WHOQOL-BREF (Figure 1).
When compared the DASS 21 scores before and after the OM chanting (44.36 ±12.32 to 21.45± 9.56) improvement in the psychological level and sleep quality (11.24± 3.89 to 6.70± 3.51) was observed (Table 2).
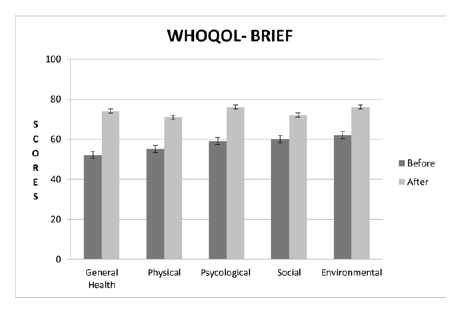
Figure 1.
Comparison of Quality of Life before and after OM.
| Variables | Before intervention | After intervention | P value |
|---|---|---|---|
| Total DASS-21 | 44.36 ±12.32 | 21.45± 9.56 | 0.01 |
| Depression level | 13.26±4.52 | 7.84±3.96 | 0.01 |
| Anxiety level | 14.38±5.28 | 8.29±4.73 | 0.05 |
| Stress level | 16.88±4.90 | 7.32±3.91 | 0.05 |
| PSQI level | 11.24± 3.89 | 6.70± 3.51 | 0.03 |
DISCUSSION
COVID-19 patients under home quarantine experienced poor sleep quality and psychological distress as noted by the PSQI and DASS scores in our study. OM chanting was known to deactivate the prefrontal cortex11
(SEKAR et al., 2019) and other brain areas (amygdala, anterior cingulate gyrus, hippocampus, insula, orbitofrontal cortex, parahippocampalgyrus and thalamus) which is usually activated during stress and depression7
(Kalyani et al., 2011). Further, the chanting of OM was found to improve parasympathetic dominance which along with the specific cortical deactivation could have reduced the stress, depression and anxiety levels of the COVID patients12 (Telles et al., 1995). Regular chanting of OM was found to be effective in increasing the sleep quality by increasing the alpha waves in EEG which corroborates with our findings13 (Anand, 2014) and deactivation of the sympathetic nervous system.14–15 The significant changes in the level of cortisol, inhibition of sympathetic nervous system along with reduced stress, anxiety and depression scores could have resulted in the positive changes of sleep pattern and overall improvement in the quality of life as observed in our study.16
Thus OM chanting has been effective in inducing these changes in the brain and regulates the autonomic nervous system and increases the relaxation response. This helps in altering the perception of stress thereby calming the mind, reducing the psychological distress and helps in improve the quality of sleep and life in COVID-19 patients in home isolation. The absence of the control group and smaller sample would be the limitations. As the practice of OM meditation was found to be beneficial, it can be used as an adjuvant therapy for alleviating psychological symptoms in COVID-19 patients undergoing home isolation. Further multicentric clinical trials with longer duration are needed to substantiate our findings on improving psychological symptoms in COVID-19 patients.
CONCLUSION
The present study indicates that the practice of OM chanting may effectively reduce stress, anxietyand depression in isolated COVID-19 home care patients with overall improvement in sleep quality. Inculcatingthis into daily life practice for the Covid home care patients may help in bringing down the psychological problems and improving the sleep quality.
Cite this article
Rajagopalan A, Kuppusamy M, Gandhi TS. Meditation Alleviates Psychological Distress and Sleep Quality in COVID-19 Patients during Home Isolation. J Young Pharm. 2022;14(4):441-3.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
References
- World Health Organization. Origin of SARS-CoV-2. World Health Organization. 2020 [Google Scholar]
- Grover S, Dua D, Sahoo S, Mehra A, Nehra R, Chakrabarti S, et al. Why all COVID-19 hospitals should have mental health professionals: The importance of mental health in a worldwide crisis!. Asian J Psychiatr. 2020;51:102147 [PubMed] | [CrossRef] | [Google Scholar]
- Stefana A, Youngstrom EA, Hopwood CJ, Dakanalis A. The COVID-19 pandemic brings a second wave of social isolation and disrupted services. Eur Arch Psychiatry Clin Neurosci. 2020;270(6):785-6. [PubMed] | [CrossRef] | [Google Scholar]
- Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology. 2017;86:152-68. [PubMed] | [CrossRef] | [Google Scholar]
- Morgan N, Irwin MR, Chung M, Wang C. The effects of mind-body therapies on the immune system: meta-analysis. Plos One. 2014;9(7):e100903 [PubMed] | [CrossRef] | [Google Scholar]
- Kalyani BG, Venkatasubramanian G, Arasappa R, Rao NP, Kalmady SV, Behere RV, et al. Neurohemodynamic correlates of ’OM’ chanting: A pilot functional magnetic resonance imaging study. Int J Yoga. 2011;4(1):3-6. [PubMed] | [CrossRef] | [Google Scholar]
- Gomez F. A guide to the depression, anxiety and stress scale (DASS 21). Cent East Sydney Prim Health Netw. 2016 [PubMed] | [CrossRef] | [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [PubMed] | [CrossRef] | [Google Scholar]
- World Health Organization. WHOQOL-bref: Introduction, administration, scoring and generic version of the assessment: Field trial version. World Health Organization. 1996 [PubMed] | [CrossRef] | [Google Scholar]
- Sekar L, Niva W, Maheshkumar K, Thangavel G, Manikandan A, Silambanan S, et al. Effect of Mahamantra chanting on autonomic and cognitive functions-an interventional study. J Clin Diagn Res. 2019;13(5) [CrossRef] | [Google Scholar]
- Telles S, Nagarathna R, Nagendra HR. Autonomic changes during “OM” meditation. Indian J Physiol Pharmacol. 1995;39(4):418-20. [PubMed] | [Google Scholar]
- Anand H. Effect of meditation (”OM” chanting) on alpha EEG and galvanic skin response: Measurement of an altered state of consciousness. Indian J Posit Psychol. 2014;5(3):255 [PubMed] | [Google Scholar]
- Metri K, Bapat R, Vaidya M. Pre-post study of efficacy of Aum chanting on insomnia in elderly urban female population of thane city. Int J Womens Health Gynecol. 2020;2(1):114 [PubMed] | [Google Scholar]
- Vempati RP, Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90(2):487-94. [PubMed] | [CrossRef] | [Google Scholar]
- Koopman C, Nouriani B, Erickson V, Anupindi R, Butler LD, Bachmann MH, et al. Sleep disturbances in women with metastatic breast cancer. Breast J. 2002;8(6):362-70. [PubMed] | [CrossRef] | [Google Scholar]
