ABSTRACT
Background
This observational, prospective cross-sectional study aimed to assess the safety and efficacy of metoprolol and bisoprolol in the treatment of Coronary Artery Disease (CAD) patients.
Materials and Methods
The study received institutional ethics approval and was conducted at a tertiary care private teaching hospital over six months. Ninety CAD patients were included, with demographics and clinical characteristics recorded. Vital signs were measured at baseline, 48 hr, 7 days, and 1 month. Angina severity was assessed using the Canadian Cardiovascular Society Grading Scale and New York Heart Association classification. Statistical analysis compared outcomes between metoprolol and bisoprolol groups.
Results
Male patients (72.22%) received metoprolol more frequently, while bisoprolol was preferred among females (28.88%). Age had minimal influence on medication choice. Metoprolol-treated patients had higher Left Ventricular Ejection Fraction (LVEF) values (50.26%) compared to bisoprolol-treated patients (45.78%). Regional Wall Motion Abnormalities (RWMA) was similar between groups. Both medications effectively reduced hypertension severity and vital parameters, with significant reductions in Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and Heart Rate (HR) with metoprolol. The prevalence of chest pain decreased in both groups, with Class III patients achieving complete relief. Breathlessness symptoms improved overall, with some patients experiencing relief while others showed reduced symptoms. Side effects were low in both groups, but metoprolol had a slightly higher incidence.
Conclusion
Metoprolol and bisoprolol demonstrated safety and efficacy in managing CAD patients. Metoprolol showed advantages in LVEF improvement and greater reduction in SBP, DBP, and HR, but it had a slightly higher side effect incidence. Both medications effectively alleviated chest pain and breathlessness symptoms. This study provides valuable insights into the clinical characteristics and outcomes associated with metoprolol and bisoprolol in CAD patients, supporting their use in managing cardiac symptoms and hypertension.
INTRODUCTION
Non-communicable diseases, which commonly include Cardiovascular Disease (CVD), various types of cancer, chronic respiratory disorders, diabetes, and more, collectively account for roughly 60% of all deaths. Specifically, within this group, conditions such as ischemic heart disease and cerebrovascular incidents like strokes are responsible for 17.7 million fatalities and represent the leading causes.1 As per the World Health Organization, India bears a substantial share of worldwide mortality, especially among younger age groups, contributing to approximately 20% of these deaths. The results from the Global Burden of Disease study indicate an age-adjusted CVD mortality rate of 272 per 100,000 individuals in India, which is significantly greater than the global average of 235. Significantly, CVD tend to afflict Indians nearly a decade earlier than their counterparts in Western populations.2 Within the Indian population, there are several concerning aspects related to CVD, including its early onset, rapid progression, and increased mortality rates. Indians are renowned for having the highest prevalence of CAD, and the usual risk factors do not completely explain this heightened risk. Furthermore, there is a deficiency in structured data collection methods to monitor cardiac mortality and morbidity in the Indian subcontinent. Additionally, a notable percentage of deaths happen in people’s homes, often without a clear understanding of the exact cause of death. In 2016, in India, CVD were responsible for 28.1% of all reported fatalities and 14.1% of the overall burden measured in Disability-Adjusted Life Years (DALYs). This marks a notable contrast to the statistics from 1990 when CVD constituted 15.2% of total deaths and 6.9% of total DALYs.3 Another significant concern within India’s array of CVD is the presence of hypertensive heart disease, which led to 261,694 fatalities in 2013. This marks a substantial rise of 138% compared to the statistics documented in 1990. In India, the prevalence of Coronary Artery Disease (CAD) is 21.4% among individuals with diabetes and 11% among those without diabetes. Additionally, CAD is about half as common in rural areas of the country compared to urban populations.4 Since the inception of β-adrenergic receptor blockers (commonly known as β-blockers) in the 1960s for treating angina, their utilization has significantly risen in the management of various heart-related conditions. Beta-blockers are regarded as the foremost option for long-term pharmaceutical management in individuals with coronary artery disease, supported by favourable evidence demonstrating their effectiveness in enhancing clinical results for patients with acute myocardial infarction5,6 or heart failure.7 Medications like acebutolol, atenolol, bisoprolol, esmolol, metoprolol, and nebivolol fall under the category of cardio-selective beta-blockers. However, only specific cardio selective beta-blockers approved by the Food and Drug Administration are utilized for the treatment of various medical conditions. However, recent hypertension treatment guidelines have positioned beta-blockers as a secondary option, giving preference to other antihypertensive drugs like angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers, unless a patient has a compelling reason, such as CAD or heart failure, that warrants their use. This is primarily because beta-blockers exert a more significant impact on heart rate rather than on the tone of blood vessels, as mentioned earlier.8 In recent times, there has been ongoing discussion and debate regarding the application of beta-blockers for treating all individuals with CAD. The study aims to determine which medication exhibits stronger and more cardio-selective effects. Specifically, our research compares metoprolol and bisoprolol, both of which are beta blockers known for their cardio-selective properties. Over the years, a wide range of beta-blockers has been employed in clinical cardiology practice to achieve safety and effectiveness. This evolution has shifted from non-selective blockers to highly selective beta-blockers. While metoprolol and bisoprolol are widely used beta blockers and have been subject to numerous isolated clinical trials, there is currently no direct comparison available between them. Therefore, our study is designed as a head-to-head comparison to assess the safety and efficacy of metoprolol and bisoprolol, with the goal of improving clinical outcomes.
MATERIALS AND METHODS
The study design was an observational, prospective cross-sectional study received approval from the Institutional Ethics Committee (SVIEC/ON/Phar/BNPG20/21043) and was conducted over a period of six months at a multispecialty tertiary care private teaching hospital in Gujarat, India. Every individual involved in the study gave their written informed consent. The study strictly adhered to principles of anonymity, confidentiality, and professional secrecy for all participants. In accordance with the guidance provided by the statistician, total of 90 participants were suggested in the study. Participants who met the inclusion criteria, such as being 18 years or older and having a confirmed diagnosis of stable or unstable angina, chest pain, myocardial infarction, as well as a previous history of acute coronary syndrome, were included in the study. Those who met the exclusion criteria, including patients with cardiovascular shock, COPD, bradycardia, and those who did not provide consent, were not included in the study. The process of gathering data entailed utilizing a pre-established form designed for capturing details pertaining to patient demographics, social background, diagnosis, disease duration, vital signs, laboratory results, and clinical outcomes. We recorded vital signs at multiple time intervals, including day 0 as the baseline, after 48 hr as the short-term assessment, after 7 days, and 1 month as the mid-term evaluation, in order to evaluate the safety and effectiveness of metoprolol and bisoprolol treatment. The severity of angina was gauged using the Canadian Cardiovascular Society Grading Scale and the New York Heart Association classification. Subsequently, a statistical analysis was conducted to determine the efficacy and safety of metoprolol and bisoprolol in the treatment of CAD patients. This analysis involved using appropriate statistical tests to examine differences in clinical outcomes between the two treatment groups.
RESULTS
Demographic attributes of patients
In our research, we included a total of 90 CAD patients from the Cardiac ICCU. Among these participants, 25 (27.77%) were female, while 65 (72.22%) were male. Within the female group, 12 (26.66%) were prescribed metoprolol, and 13 (28.88%) were prescribed bisoprolol. In the male cohort, 33 (73.33%) were on metoprolol, and 32 (71.11%) were on bisoprolol. The average age of patients receiving metoprolol was 51.51, with a Standard Deviation (SD) of 15.37, whereas patients receiving bisoprolol had an average age of 52.33, with an SD of 13.09.
The patients were divided into three age groups, as outlined in Table 1. In the 41-50 age group, 12 (26.66%) were prescribed metoprolol, and 13 (28.88%) were prescribed bisoprolol. Among those aged 51-60, 11 (24.44%) were taking metoprolol, while 8 (17.77%) were taking bisoprolol. For patients over the age of 61, 12 (26.66%) were on metoprolol, and 14 (31.11%) were on bisoprolol. Additionally, the study provides insights into the patients’ residential areas. Among the 45 patients receiving metoprolol, 28 (62.22%) resided in rural areas, while 17 (37.77%) lived in urban areas. In the case of the 45 patients receiving bisoprolol, 23 (51.11%) hailed from rural areas, and 22 (48.88%) were from urban locations (Table 1).
| Years | Drugs | Total patients (n=90) | |
|---|---|---|---|
| Metoprolol (n=45) | Bisoprolol (n=45) | ||
| Age | |||
| 18-25 | 4 (8.88) | 1 (2.22) | 5 (5.55) |
| 26-30 | 2 (4.44) | 1 (2.22) | 3 (3.33) |
| 31-35 | 0 (0) | 4 (8.88) | 4 (4.44) |
| 36-40 | 4 (8.88) | 4 (8.88) | 8 (8.88) |
| 41-50 | 12 (26.66) | 13 (28.88) | 25 (27.77) |
| 51-60 | 11 (24.44) | 8 (17.77) | 19 (21.11) |
| > 61 | 12 (26.66) | 14 (31.11) | 26 (28.88) |
| Gender | |||
| Male | 33 (73.33) | 32 (71.11) | 65 (72.22) |
| Female | 12 (26.66) | 13 (28.88) | 25 (27.77) |
| Residence | |||
| Rural | 28 (62.22) | 23 (51.11) | 51 (56.66) |
| Urban | 17 (37.77) | 22 (48.88) | 39 (43.33) |
Mean LVEF and RMWA of participants
This pertains to the average Left Ventricular Ejection Fraction (LVEF) among patients prescribed either metoprolol or bisoprolol. LVEF is a measure indicating the percentage of blood ejected from the heart’s left ventricle during each heartbeat. In the metoprolol group, comprising 45 participants, the average LVEF was 50.26% with a SD of 9.89%. Conversely, in the bisoprolol group, which also had 45 participants, the mean LVEF was 45.78% with an SD of 9.31%. This pertains to how patients are categorized depending on the presence or absence of Regional Wall Motion Abnormalities (RWMA), which serves as an indicator of heart muscle damage. In the group treated with metoprolol, 64.44% of patients had negative RWMA, while 35.55% had positive RWMA. In the bisoprolol group, which included 45 participants, 55.6% showed negative RWMA, and 44.4% displayed positive RWMA (Figure 1).

Figure 1:
Mean LVEF and RMWA of participants.
JNC 8 classification of blood pressure after treatment of beta blockers
The patients were categorized based on their blood pressure readings according to the JNC 8 guidelines. The statement provides details about the number of patients in each group who had Stage 1 or Stage 2 Hypertension (HTN) at the beginning and how their blood pressure readings changed during a one-month follow-up period. In the metoprolol group, consisting of 45 participants, 20 had Stage 1 HTN at the beginning, and this number decreased to 4 after one month. The remaining patients shifted to the pre-hypertensive stage, with 19 patients at baseline increasing to 38 after one month. In the bisoprolol group, also comprising 45 participants, 22 had Stage 2 HTN initially, and this number decreased to 3 after one month. The remaining patients shifted to Stage 1 HTN, with 19 patients at baseline increasing to 34 after one month (Table 2).
| JNC 8 classification of blood pressure after metoprolol | |||||
|---|---|---|---|---|---|
| Stage | Baseline | 48 hr | 7th day | 1 month | Statistical test |
| Normal | 03 | 03 | 03 | 02 | Chi-square for trend: 23.89, df:09, P:0.004 |
| Pre-hypertension | 19 | 30 | 35 | 38 | |
| State I HTN | 20 | 10 | 06 | 04 | |
| Stage II HTN | 03 | 02 | 01 | 01 | |
| JNC 8 classification of blood pressure after bisoprolol | |||||
| Normal | 01 | 01 | 01 | 01 | Chi-square for trend: 28.43, df:09, P:0.0008 |
| Pre-hypertension | 03 | 03 | 10 | 07 | |
| State I HTN | 19 | 27 | 27 | 34 | |
| Stage II HTN | 22 | 14 | 07 | 03 | |
Comparative analysis of Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and Heart Rate (HR) during post-metoprolol follow-up visits in patients
Throughout the study, significant changes in vital parameters were observed. Initially, at baseline, SBP was measured at 136.40±14.42 mmHg, DBP at 80.26±7.64 mmHg, and HR at 80.73±9.81 beats per minute. However, on Day 2, these values started to show a decline, with SBP decreasing to 134.08±13.68 mmHg, DBP to 78.40±7.37 mmHg, and HR to 79.95±9.01 beats per minute. Subsequently, by Day 7, further reductions were evident, with SBP averaging 130.73±12.13 mmHg, DBP at 76.44±5.91 mmHg, and HR at 78.53±7.25 beats per minute. These trends persisted after 1 month of metoprolol treatment, resulting in SBP measurements of 130.40±11.09 mmHg, DBP at 76.51±5.07 mmHg, and HR at 75.11±8.16 beats per minute. The highly significant differences indicated by Friedman’s two-way analysis of variance by ranks (p<0.0001) underscore the noteworthy impact of metoprolol on SBP, DBP, and HR over the study’s duration (Table 3).
| Metoprolol | Baseline | Day 2 | Day 7 | 1 month |
|---|---|---|---|---|
| SBP (mmHg) | 136.40 ± 14.42 | 134.08 ± 13.68 | 130.73 ± 12.13 | 130.40 ± 11.09 |
| DBP (mmHg) | 80.26 ± 7.64 | 78.40 ± 7.37 | 76.44 ± 5.91 | 76.51 ± 5.07 |
| HR | 80.73 ± 9.81 | 79.95 ± 9.01 | 78.53 ± 7.25 | 75.11 ± 8.16 |
Comparative analysis of chest pain and breathlessness during post-metoprolol follow-up visits in patients
The Figure 2 illustrates the prevalence of chest pain among patients categorized into three classes: Class I, Class II, and Class III. At the baseline assessment, 12 patients (26.66%) in Class I reported chest pain, while Class II had 25 patients (55.55%) with chest pain, and Class III had 8 patients (17.77%) experiencing chest pain. After one month of observation, there was a notable shift in the prevalence of chest pain, with 33 patients (73.33%) in Class I reporting it, while only 12 patients (26.66%) in Class II continued to experience chest pain. Interestingly, there were no reports of chest pain in Class III after the one-month follow-up period. These findings suggest dynamic changes in the occurrence of chest pain among the different classes of patients over time.
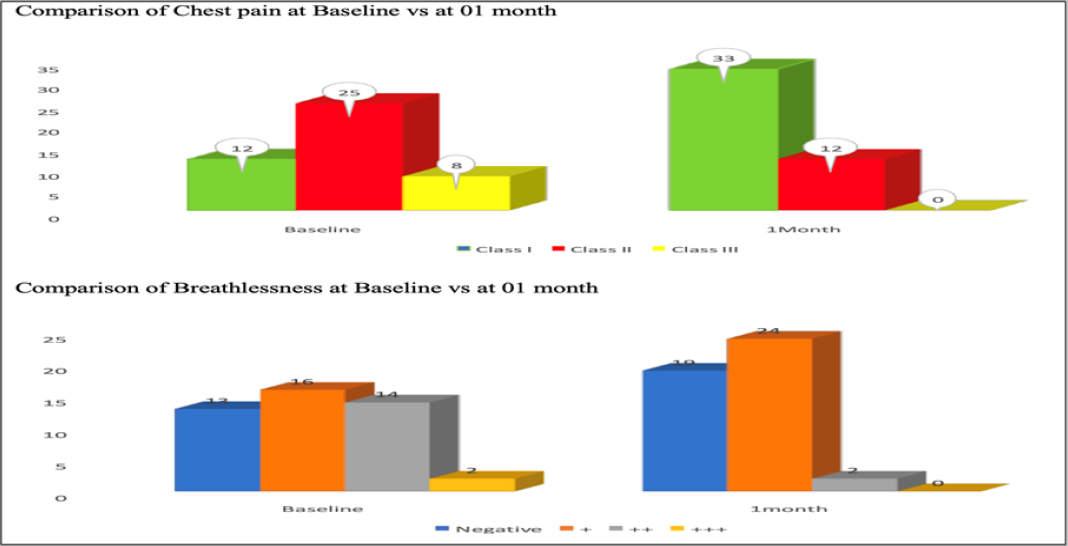
Figure 2:
Comparing chest pain and breathlessness in post-metoprolol follow-up visits.
The research closely monitored breathlessness symptoms in patients and uncovered significant fluctuations over time. Initially, during the baseline assessment, a substantial portion of patients reported mild breathlessness (35.55%) and moderate breathlessness (31.11%), while a small fraction experienced severe breathlessness (4.44%). Conversely, nearly a third of the patients exhibited no signs of breathlessness (28.88%). Following a one-month observation period, there was a remarkable shift in these symptoms. Mild breathlessness showed a substantial increase, reaching 53.33%, whereas the prevalence of moderate breathlessness plummeted to a mere 4.44%, and no instances of severe breathlessness were reported. Encouragingly, a significant proportion of patients (42.22%) reported no breathlessness symptoms, indicating an overall improvement in their condition. These findings underscore the dynamic nature of breathlessness symptoms, with some patients experiencing relief while others demonstrated a worsening of symptoms during the study duration (Figure 2).
Comparative analysis of SBP, DBP and HR during post-bisoprolol follow-up visits in patients
The study tracked vital parameter changes in patients treated with bisoprolol at various time points, revealing significant trends. Initially, at baseline, patients exhibited elevated levels, with SBP at 154.40±15.54 mmHg, DBP at 83.80±9.62 mmHg, and HR at 84.84±7.68 beats per minute. By Day 2, there was a noticeable reduction in these parameters, with SBP decreasing to 150.86±13.70 mmHg, DBP to 80.20±9.09 mmHg, and HR to 82.24±7.45 beats per minute. Subsequently, on Day 7, further reductions were observed, with SBP averaging 145.80±13.95 mmHg, DBP at 76.42±8.23 mmHg, and HR at 79.75±6.89 beats per minute. The trend continued after 1 month of bisoprolol treatment, resulting in SBP measurements of 142.93±11.24 mmHg, DBP at 74.02±8.27 mmHg, and HR at 75.86±6.18 beats per minute. The highly significant difference indicated by Friedman’s two-way analysis of variance by ranks (p<0.0001) underscores the substantial impact of bisoprolol on SBP, DBP, and HR throughout the study, highlighting its efficacy in managing these vital parameters (Table 4).
| Bisoprolol | Baseline | Day 2 | Day 7 | 1 month |
|---|---|---|---|---|
| SBP (mmHg) | 154.40 ± 15.54 | 150.86 ± 13.70 | 145.80 ± 13.95 | 142.93 ± 11.24 |
| DBP (mmHg) | 83.80 ± 9.62 | 80.20 ± 9.09 | 76.42 ± 8.23 | 74.02 ± 8.27 |
| HR | 84.84 ± 7.68 | 82.24 ± 7.45 | 79.75 ± 6.89 | 75.86 ± 6.18 |
| Friedman’s two-way analysis of variance by ranks P:0.0001 | ||||
Comparative analysis of chest pain and breathlessness during post-bisoprolol follow-up visits in patients
The Figure 3 illustrates how patients responded to bisoprolol treatment for chest pain at baseline and after one month. Initially, the distribution across different classes (Class I, Class II, Class III) varied, with 8 patients in Class I, 20 in Class II, 17 in Class III, and none reporting no chest pain. However, after one month of treatment, a significant shift occurred, with 34 patients classified as Class I, 10 in Class II, none in Class III, and only 1 patient reporting no chest pain. This indicates a substantial reduction in chest pain, particularly noteworthy in Class III patients who experienced complete relief from this symptom. Bisoprolol demonstrated its efficacy in managing chest pain during the study period.
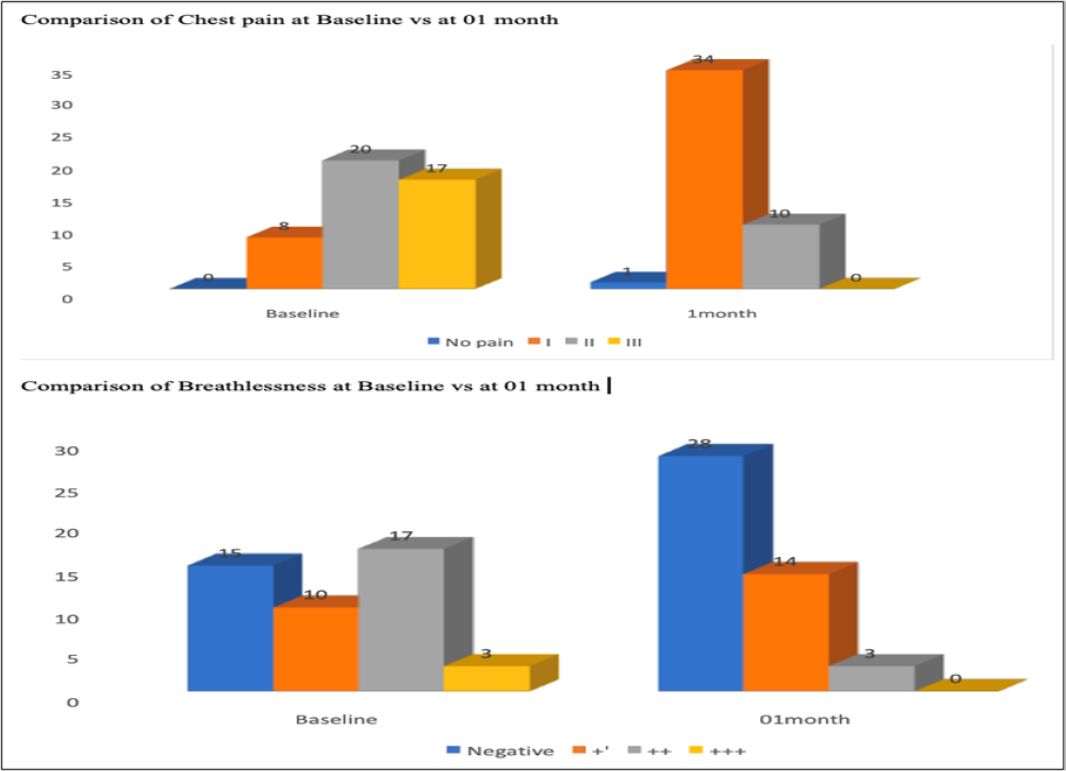
Figure 3:
Comparing chest pain and breathlessness in post-bisoprolol follow-up visits.
The prevalence of breathlessness among patients at baseline and after one month of observation. Initially, 10 patients reported mild breathlessness (+), 17 had moderate breathlessness (++), and 3 experienced severe breathlessness (+++), while 15 patients were free of breathlessness symptoms (Negative). After one month, the pattern shifted significantly. The count of patients with mild breathlessness increased to 14, while the number of those with moderate breathlessness decreased to 3. Remarkably, there were no reports of severe breathlessness (+++). Moreover, 28 patients exhibited no breathlessness symptoms, indicating an overall improvement in this symptom during the one-month follow-up. These results highlight the dynamic nature of breathlessness symptoms, with some patients finding relief while others showed a reduction in their symptoms over the observation period (Figure 3).
Adverse drug reactions during metoprolol and bisoprolol treatment
The Table 5 compares the side effects observed in patients treated with metoprolol (n=45) and bisoprolol (n=45) along with their respective frequencies. In the metoprolol group, the most common side effect was palpitation and chest discomfort, affecting 8.88% of patients, while 17.77% experienced side effects in total. Conversely, in the bisoprolol group, 11.11% patients experienced side effects. These results provide insight into the side effect profiles of metoprolol and bisoprolol, with metoprolol showing a slightly higher incidence of side effects in this patient sample.
| Metoprolol (n=45) | Bisoprolol (n=45) | ||
|---|---|---|---|
| Side effects | Frequency | Side effects | Frequency |
| Palpitation and Chest discomfort. | 04 (8.88%) | Dizziness and Chest Discomfort. | 01 (2.22%) |
| Fatigue and Somnolence. | 02 (4.44%) | Headache and Constipation. | 01 (2.22%) |
| Chest discomfort and Fatigue. | 01 (2.22%) | Dizziness. | 01 (2.22%) |
| Chest discomfort and Somnolence. | 01 (2.22%) | Abdominal discomfort and palpitation. | 01 (2.22%) |
| Loss of appetite. | 01 (2.22%) | ||
| Total | 8 (17.77%) | Total | 5 (11.11%) |
DISCUSSION
The patient’s age plays a significant role in the development, duration, and severity of hypertension. In essential hypertension, the regulation of sympathetic cardiovascular function undergoes a transition. Initially, there are heightened responses through beta-adrenoceptor, leading to increased cardiac output and renin levels. Later on, there is a shift towards blunted responses and a predominance of alpha-adrenoceptor-mediated vasoconstriction, accompanied by higher intracellular levels of sodium and calcium. This understanding of the pathophysiology informs treatment approaches, with younger patients, often exhibiting elevated renin levels, benefiting from beta-blockers or converting-enzyme inhibitors. Conversely, older patients, typically with lower renin levels, show favorable responses to calcium entry blockers. This offers a fresh perspective on managing hypertension and the potential for cardioprotective effects.9 However, our research demonstrates that older individuals can also derive advantages from beta-blockers. The present study involved a comparison of two specific beta-blockers, namely metoprolol and bisoprolol, when administered to patients with hypertension. In our research, we conducted a comprehensive analysis of 90 CAD patients admitted to the Cardiac ICCU, shedding light on various aspects of their demographics and clinical characteristics. Among these patients, the gender distribution revealed that 27.77% were female, while the majority, constituting 72.22%, were male. Further examination within gender subgroups showed that a comparable proportion of females were prescribed metoprolol (26.66%) and bisoprolol (28.88%). In contrast, the majority of male patients were on metoprolol (73.33%) and bisoprolol (71.11%). We also explored the average ages of patients receiving these medications, with those on metoprolol having an average age of 51.51 and those on bisoprolol averaging 52.33. Furthermore, we categorized patients into different age groups, revealing variations in medication prescriptions. In the 41-50 age groups, both metoprolol and bisoprolol were prescribed relatively evenly. However, among patients aged 51-60, metoprolol was more commonly prescribed, while for patients over 61, bisoprolol had a higher prevalence. We also considered patients’ residential areas, indicating that both medications were administered to individuals residing in both rural and urban settings. Our study delved into the vital clinical parameter of LVEF, a critical measure of heart function. While both metoprolol and bisoprolol were effective, there was a slight difference in their impact, with metoprolol patients having an average LVEF of 50.26% and bisoprolol patients averaging 45.78%. We also explored RWMA as an indicator of heart muscle damage. The analysis showed that metoprolol and bisoprolol had similar effectiveness in this regard, with the majority of patients in both groups having negative RWMA, but there were some patients with positive RWMA, indicating continued challenges. Additionally, we considered blood pressure control and observed changes in hypertension staging according to JNC 8 guidelines. Both metoprolol and bisoprolol had a positive impact on hypertension management, with patients transitioning to lower stages of hypertension or even pre-hypertensive categories. These findings align with a prior investigation in which the study concentrated on primary prevention in middle-aged white males, assessing the impacts of initiating antihypertensive treatment with metoprolol versus thiazide diuretics. Over a median observation period of 4.2 years, metoprolol demonstrated a notable decrease in overall mortality in comparison to thiazide diuretics, primarily attributable to a reduction in fatalities stemming from coronary heart disease and stroke.10 Our findings received additional support from another study, which included 2,418 patients. Of these, 2,161 were enrolled, and the majority were men (66.64%) with an average age of 51.7 years, including 19.19% smokers. This study also observed a significant decrease in systolic and diastolic blood pressure as well as heart rate. The median bisoprolol dose was 5 mg/day and was found to be well-tolerated up to 10 mg/day. Adverse events, which affected 1.9% of patients, were generally mild to moderate in severity, and none necessitated discontinuation of treatment.11 Finally, we closely monitored vital parameters such as SBP, DBP and HR over the course of the study. These parameters showed consistent and significant reductions over time, highlighting the efficacy of metoprolol and bisoprolol in controlling these vital signs. Bisoprolol produced a more pronounced decrease in PR (pulse rate), enhanced BRS (baroreflex sensitivity), and reduced vascular stiffness. Bisoprolol may be valuable for hypertensive patients with cardiac or vascular conditions characterized by advanced atherosclerosis and heightened sympathetic nervous system activity.12 Canadian Cardiovascular Society Angina (CCSA) classes I to III showed an inverse correlation with Duke Activity Status Index (DASI) scores and exhibited a linear relationship with mortality. The resemblance in outcomes among patients in class III and IV can likely be attributed to the influence of the stability of their symptoms, introducing a potential confounding factor. The increased mortality risk observed in class III and IV patients with an unstable symptom course underscores the need for a revised CCSA definition that takes this factor into account. Furthermore, we assessed the prevalence of chest pain and breathlessness among patients, categorizing them into different classes.13 In current study, The impact of bisoprolol treatment on chest pain was assessed both at baseline and after one month. Initially, patients were distributed across different classes (Class I, Class II, Class III), with 8 in Class I, 20 in Class II, 17 in Class III, and none reporting no chest pain. However, after one month of treatment, a significant transformation occurred, with 34 patients categorized as Class I, 10 in Class II, none in Class III, and only 1 patient reporting no chest pain. This highlights a substantial reduction in chest pain, particularly noteworthy for Class III patients who achieved complete relief from this symptom. Bisoprolol demonstrated its effectiveness in managing chest pain during the study period. It’s important to note that an increase in CCSA class signifies greater severity and is associated with higher mortality. Conversely, Metoprolol also demonstrated effectiveness in reducing chest pain. During the initial assessment, 12 patients (26.66%) in Class I reported chest pain, while Class II had 25 patients (55.55%) with chest pain, and Class III had 8 patients (17.77%) experiencing chest pain. However, after one month of observation, a significant shift in the prevalence of chest pain was observed, with 33 patients (73.33%) in Class I reporting it, while only 12 patients (26.66%) in Class II continued to experience chest pain. Notably, there were no reports of chest pain in Class III after the one-month follow-up period. These findings indicate dynamic changes in the occurrence of chest pain among the various patient classes over time. Lastly, we examined the side effect profiles of metoprolol and bisoprolol. While both medications were generally well-tolerated, metoprolol showed a slightly higher incidence of side effects in our patient sample.
CONCLUSION
In our study of 90 CAD patients from the Cardiac ICCU, we observed distinct patterns between metoprolol and bisoprolol treatment. Notably, metoprolol was more frequently prescribed to male patients, while bisoprolol was relatively more common among female patients. Patients across different age groups received either medication, and age appeared to have minimal influence on medication choice. Interestingly, metoprolol-treated patients exhibited higher LVEF values than those treated with bisoprolol, which might be indicative of better cardiac function with metoprolol. RWMA were relatively similar between the two groups. When categorizing patients by blood pressure levels, both medications showed effectiveness in reducing hypertension severity over one month. Vital parameters like systolic blood pressure SBP, DBP, and HR demonstrated significant reductions with metoprolol treatment. The prevalence of chest pain and breathlessness symptoms fluctuated over time, with both medications proving effective in alleviating these symptoms. Importantly, while side effects were relatively low with both medications, metoprolol exhibited a slightly higher incidence of side effects than bisoprolol. Overall, this study provides valuable insights into the clinical characteristics and outcomes associated with metoprolol and bisoprolol in CAD patients, underscoring their efficacy in managing cardiac symptoms and hypertension.
Cite this article
Maheshwari R, Rathi P, Shah J, Patel R, Mathew C, Rajput H, et al. Metoprolol and Bisoprolol in Coronary Artery Disease: An Observational Prospective Cross-Sectional Study. J Young Pharm. 2024;16(1):42-9.
ACKNOWLEDGEMENT
We are sincerely thankful to Sumandeep Vidyapeeth (Deemed to be University) for providing support to carry out the study.
ABBREVIATIONS
| CAD | Coronary Artery Disease |
|---|---|
| CCSA | Canadian Cardiovascular Society Angina |
| CVD | Cardiovascular Disease |
| DALYs | Disability-Adjusted Life Years |
| DASI | Duke Activity Status Index |
| DBP | Diastolic Blood Pressure |
| HR | Heart Rate |
| HTN | Hypertension |
| ICCU | Intensive Coronary Care Unit |
| LVEF | Left Ventricular Ejection Fraction |
| RWMA | Regional Wall Motion Abnormalities |
| SBP | Systolic Blood Pressure |
| SD | Standard Deviation |
References
- WHO. Global health estimates 2015: deaths by cause, age, sex, by country and by region. 2016:2000-15.
- Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133(16):1605-20. [PubMed] | [CrossRef] | [Google Scholar]
- Ruhil R. India has reached on the descending limb of tobacco epidemic. Indian J Community Med. 2018;43(3):153-6. [PubMed] | [CrossRef] | [Google Scholar]
- Sreeniwas Kumar AS, Sinha N. Cardiovascular disease in India: a 360 degree overview. Med J Armed Forces India. 2020;76(1):1-3. [PubMed] | [CrossRef] | [Google Scholar]
- Puymirat E, Riant E, Aissaoui N, Soria A, Ducrocq G, Coste P, et al. β-blockers and mortality after myocardial infarction in patients without heart failure: multicentre prospective cohort study. BMJ. 2016;354:i4801 [PubMed] | [CrossRef] | [Google Scholar]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-77. [PubMed] | [CrossRef] | [Google Scholar]
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, et al. 2017 ACC/ AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137-61. [PubMed] | [CrossRef] | [Google Scholar]
- Khan O, Patel M, Tomdio AN, Beall J, Jovin IS. Beta-blockers in the prevention and treatment of ischemic heart disease: evidence and clinical practice. Heart Views. 2023;24(1):41-9. [PubMed] | [CrossRef] | [Google Scholar]
- Bühler FR. Age and cardiovascular response adaptation. Determinants of an antihypertensive treatment concept primarily based on beta-blockers and calcium entry blockers. Hypertension. 1983;5(2):III94-100. [PubMed] | [CrossRef] | [Google Scholar]
- Wikstrand J, Warnold I, Olsson G, Tuomilehto J, Elmfeldt D, Berglund G, et al. Primary prevention with metoprolol in patients with hypertension: mortality results from the MAPHY study. JAMA. 1988;259(13):1976-82. [PubMed] | [CrossRef] | [Google Scholar]
- Channaraya V, Marya RK, Somasundaram M, Mitra D, Tibrewala KD, BRIGHT investigators, et al. Efficacy and tolerability of a β-1 selective β blocker, bisoprolol, as a first-line antihypertensive in Indian patients diagnosed with essential hypertension (BRIGHT): an open-label, multicentric observational study. BMJ Open. 2012;2(3):e000683 [PubMed] | [CrossRef] | [Google Scholar]
- Eguchi K, Hoshide S, Kario K. Effects of celiprolol and bisoprolol on blood pressure, vascular stiffness, and baroreflex sensitivity. Am J Hypertens. 2015;28(7):858-67. [PubMed] | [CrossRef] | [Google Scholar]
- Kaul P, Naylor CD, Armstrong PW, Mark DB, Theroux P, Dagenais GR, et al. Assessment of activity status and survival according to the Canadian Cardiovascular Society angina classification. Can J Cardiol. 2009;25(7):e225-31. [PubMed] | [CrossRef] | [Google Scholar]
