ABSTRACT
Hypothyroidism is a chronic condition with an underactive thyroid gland. The thyroid gland produces thyroid hormones mainly, thyroxine (T4) and triiodothyronine (T3). Women are more at risk of hypothyroidism than men. The symptoms of hypothyroidism are not specific. A blood test to measure thyroid hormones should be needed for the diagnosis of hypothyroidism. The mild cognitive symptoms associated with hypothyroidism are difficult to detect in the early stages in adults. But in elderly patients, it can be easily detected. Memory is the most common cognitive domain affected in elderly hypothyroid patients. In elderly patients, the hypothyroid-impaired cognitive impairment can progress into dementia or other related complications if left untreated. Thyroid hormones have an important role in regulating metabolism. Metabolic disorders were common in hypothyroidism. Thyroid hormone supplementation with levothyroxine is the standard therapy for hypothyroidism. Levothyroxine should be taken on an empty stomach preferably in the early morning. Levothyroxine has several drug interactions. It can interact with proton pump inhibitors, calcium supplements, etc., and reduce levothyroxine’s oral absorption. Patients’ attitudes and knowledge toward the therapy have an important role in improving their clinical outcomes and quality of life.
INTRODUCTION
Hypothyroidism is a condition with an underactive thyroid gland. Mainly thyroid gland produces hormones like Triiodothyronine (T3) and Thyroxine (T4). If Hypothyroidism is left untreated it will lead to many complications. The clinical presentation of hypothyroidism varies this makes the diagnosis complicated. Hypothyroidism can be diagnosed by checking the thyroid hormone levels in the blood (Thyroid panel test). In overt hypothyroidism, the concentration of Thyroid Stimulating Hormone (TSH) will be higher and free Thyroxine (T4) values will be decreased. Overt hypothyroidism is becoming more prevalent with age. Mild or subclinical hypothyroidism is the early sign of thyroid failure, where Thyroid-stimulating Hormone (TSH) will be high and free thyroxin will be within the normal range.1
The symptoms of hypothyroidism vary it is not specific. Neurocognitive alterations (memory and concentration difficulty) followed by depression are more prevalent among these. The ability to pay attention, abstract, or solve problems may be affected through the disease period. If not treated it can progress to serious cognitive deficit and dementia.3 The common symptoms of hypothyroidism include weight gain, lethargy, fatigue, constipation, change in voice, cold intolerance, and dry skin. The symptoms may be absent in subclinical hypothyroidism.2
Thyroid dysfunction and metabolic syndrome are the most endocrine disorders. Metabolic syndrome is common in Hypothyroidism patients, especially in subclinical hypothyroidism. As per the National Cholesterol Education Program – Adult Treatment Panel III (NCEP-ATP III) the metabolic syndrome is present if three or more of the subsequent five criteria are met: waist circumference over 40 inches (men) or 35 inches (women), blood pressure over 130/85 mmHg, fasting triglyceride (TG) level over 150 mg/dl, fasting high-density lipoprotein (HDL) cholesterol level less than 40 mg/dl (men) or 50 mg/dl (women) and fasting blood glucose over 100 mg/dl. In Hypothyroidism, the production of thyroid hormones will be very less, So Hypothyroid patients experiences metabolic-related symptoms like weight gain, obesity, etc.3
The treatment is done as thyroid hormone replacement therapy, commonly using Levothyroxine. Significant improvements were seen in the life of patients who have undergone treatment with Levothyroxine previously. The treatment may have to continue for a lifetime, but dose adjustment is needed based on the thyroid hormone levels. Levothyroxine has many drug interactions, so dose adjustment or time spacing is needed when Levothyroxine therapy is continued along with these drugs (eg: Anti-diabetic medications, Proton pump inhibitors, supplements, etc.)4 Treatment helps to prevent the progression of the disease from subclinical hypothyroidism to overt hypothyroidism, also improves the neuropsychiatric signs, cognition, and somatic symptoms.2 Proper communication with the physician, medication adherence, and regular follow-up are needed to get symptomatic relief and to avoid further disease-related complications.4 The purpose of this review is to understand the metabolic and cognitive symptoms and its management in hypothyroidism.
METHODS
The current review was conducted by extensively reviewing the literature in PubMed, Scopus, and Google Scholar databases in English (from 1972 to 2021) with the search terms, hypothyroidism, hypothyroid, levothyroxine, thyroxine, cognitive impairment, dose adjustment in levothyroxine, hypothyroidism, and cognitive Impairment and metabolic syndrome. This review was prepared based on the information from research, reports, and review papers related to hypothyroidism, hypothyroidism with cognitive dysfunction, and metabolic syndrome and its management. We excluded non-English articles, letters, and comments.
Thyroid Hormones
The thyroid gland is a butterfly-shaped gland located in the anterior neck. The main hormones produced by the thyroid gland include thyroxine or tetraiodothyronine (T4) and triiodothyronine (T3). The Thyrotropin-releasing hormone (TRH), Thyroid-stimulating hormone (TSH), and Thyroxine work together to keep proper feedback mechanism and homeostasis. The functions of the thyroid hormones include increasing the basal metabolic rate, helping in growth, helping in the maturation of bone and skeletal system, maturation of nerves, regulation of growth hormone and body temperature, and influencing mood, and behavior. The thyroid hormones are lipophilic and bound to transport proteins. Around a small fraction (approximately 0.2%) of the thyroid hormone (free thyroxine) is unbound and active. The transporter proteins are thyroxine-binding globulin (TBG), Transthyretin, and albumin. Around two-thirds of the thyroxine is transported by thyroxine-binding globulin (TBG). Transthyretin transports thyroxine and retinol.5
Etiology of Hypothyroidism
Hypothyroidism is a condition that occurs due to inadequate functioning of the thyroid gland (primary hypothyroidism), insufficient stimulation by Thyroid Stimulating Hormone (TSH), from the pituitary gland (secondary hypothyroidism), or insufficient release of Thyrotropin-Releasing Hormone (TRH) from the hypothalamus (tertiary hypothyroidism).6 The causes of primary hypothyroidism include autoimmune thyroiditis, subacute granulomatous thyroiditis, acute infectious thyroiditis, and radiotherapy to the neck. The use of amiodarone, lithium-based mood stabilizers, and alpha interferons can also lead to hypothyroidism. So, monitoring of thyroid functions is required while taking these medications.
The causes of central hypothyroidism include, lesions compressing the pituitary, surgery or radiation to the pituitary, vascular disorders (subarachnoid hemorrhage), autoimmune disorders, and infiltrative disease.7
Epidemiology
Thyroid hormones play an important role in growth and metabolism. The prevalence of hypothyroidism is more common in females than in males. Prevalence of hypothyroidism in developed countries was about 4 – 5%,8,9 whereas in India it was reported to be about 10.95%.10 Also, 1 in 10 pregnant women in India suffers from Hypothyroidism.11
Clinical Presentation of Hypothyroidism
Thyroid hormones have a crucial role in regulating the body’s normal physiological functions. But, if the levels of these hormones vary, it can alter the body’s normal physiological functions. The severity of the symptoms of hypothyroidism depends on the degree of the thyroid dysfunction and the time course of the development of hypothyroidism. Most of the symptoms associated with hypothyroidism are non-specific. The common symptoms of hypothyroidism include weight gain, fatigue, poor concentration, depression, and menstrual irregularities. Symptoms of hypothyroidism differ with age and sex. In women, hypothyroidism may be presented with menstrual irregularities and infertility. While in older patients, cognitive symptoms may be dominant.12
The common electrocardiography (ECG) findings of hypothyroidism include bradycardia, flattened T-wave, and low voltage. In patients with severe hypothyroidism, pericardial effusion, pleural effusion, and hemodynamic instability were observed. The laboratory data on hypothyroidism may reveal, the associated conditions like hypernatremia, hypercapnia, hypoxia, normocytic anemia, elevated creatine kinase, and hyperprolactinemia, dyslipidemia, etc.13
Management of Hypothyroidism
The main goal in the management of hypothyroidism is to relieve symptoms, normalize the thyroid hormone level, prevent disease-related complications, and improve the quality of life.
Pharmacological Management of Sub-Clinical Hypothyroidism
Subclinical hypothyroidism is defined by an elevated Thyroid-stimulating Hormone (TSH) level with normal Thyroxine. Most patients with Subclinical Hypothyroidism will be asymptomatic. The commonly reported symptoms in Subclinical hypothyroidism patients are fatigue, muscle weakness, depression, mood swings, a decline in memory, cognition, cold intolerance, and moderate weight gain. The symptoms of subclinical hypothyroidism will not be severe while correlating with their Thyroid Stimulating Hormone (TSH) elevation. The effect of Levothyroxine therapy on relieving subclinical hypothyroidism-related symptoms remains controversial.14
Pharmacological Management of Overt Hypothyroidism
Treatment with thyroid hormone supplementation is needed in overt hypothyroidism. In elderly patients, the treatment is initiated with a low dose and it is gradually increased every 4 to 6 weeks until the Thyroid Stimulating Hormone (TSH) levels become normal. When Thyroid Stimulating Hormone (TSH) levels become stable, monitoring of Thyroid Stimulating Hormone (TSH) levels should be done yearly.15
Overt hypothyroidism is generally treated using oral thyroid hormone supplementation with synthetic Levothyroxine. The Levothyroxine will be peripherally converted into FT3. It is generally administered once daily with a dose of 1.6 mcg/kg in the elderly.15
Combinational Hormonal Supplementation Therapy in Hypothyroidism
Studies suggest that treatment with the combination of Levothyroxine and Triiodothyronine had shown some positive results in improving cognition and sensation of well-being. However, most other similar studies revealed that combinational therapy is not having any extra benefits compared with monotherapy. Clyde et al. and Walsh et al., through their study, suggested that Levothyroxine and Liothyronine combination doesn’t seem to give any extra benefit in reducing body weight, serum lipid levels, hypothyroid symptoms, or cognition compared to levothyroxine monotherapy.16,17
Management of Hypothyroidism in Pregnancy
Levothyroxine is the treatment of choice for hypothyroidism in pregnancy. Larger doses of Levothyroxine are needed for pregnant women, as there is a rapid rise in Thyroid Binding Globulin (TBG) levels during pregnancy. Women who have hypothyroidism and are on treatment with Levothyroxine need to increase their Levothyroxine doses before pregnancy. Their Levothyroxine daily doses should be increased by 30 – 50%. The full replacement Thyroxine dose is around 2 – 2.4 mcg/kg/day during the time of pregnancy. It is advised to check serum-free Thyroxine (FT4) and TSH levels every month during pregnancy. The thyroxine doses need to be titrated till the serum Thyroid Stimulating Hormone (TSH) value reaches less than 2.5 m IU/L. Follow-up every 4 to 6 weeks with free Thyroxine (FT4) levels are needed till the delivery, for Levothyroxine dose adjustments, and after the delivery, they need Levothyroxine dose reduction.18,19
Non-pharmacological Management of Hypothyroidism
Patients with hypothyroidism may need to take their medicines throughout their life. So, along with pharmacological therapy, nonpharmacological therapies are also beneficial for them. The nonpharmacological treatments include exercise, stress management, and diet.20
i) Exercise
Exercises will be helpful for hypothyroidism patients as, it improves the energy level, stimulate the secretion of thyroid hormone, and increase the tissue sensitivity to thyroid hormones. Hypothyroidism patients can do mild to moderate exercises. Walking, cycling, and practicing yoga, will be beneficial for them.20 Exercises can have an impact on thyroid hormones. Studies have shown that thyroid hormone levels (T3 and T4) were significantly improved following exercise.21
ii) Dietary Modifications
Patients with hypothyroidism should follow a diet rich in vitamins, minerals, iron, iodine, selenium, etc. They should eat foods like dairy products, eggs, fish, meats, fruits, and vegetables. But they should avoid goitrogenic foods. The intake of goitrogenic foods can be a reason for persistent goiter. The goitrogenic foods are broccoli, cabbage, cauliflower, radish, turnips, and cassava. The concentration of glucosinolates is high in cabbage and cauliflower, cyanogenic glucosides are present in cassava and bamboo shoots, and thiocyanates are present in mustard, turnip, and radish.22 Goitrogenic substances can inhibit the iodine uptake thereby reducing the activity of thyroid peroxidase enzyme and thyroid hormone synthesis.
Metabolic Syndrome in Hypothyroidism
Metabolic syndrome is a cluster of interconnected metabolic abnormalities characterized by central obesity, high triglycerides, low high-density lipoprotein cholesterol, hypertension, and hyperglycemia. Metabolic syndrome is also known as syndrome X, insulin resistance syndrome. Hyperlipidemia and obesity will increase the risk for cardiovascular disorders.22 The relation between hypothyroidism and metabolic syndrome varies. It can be influenced by age, race, and gender. Studies suggest that there is a significant difference in waist circumference in hypothyroid patients with metabolic syndrome compared with metabolic syndrome patients without thyroid dysfunction. Studies suggest that High-Density Lipoprotein (HDL) has a negative correlation with thyroid Stimulating Hormone (TSH) levels compared with Low-Density Lipoproteins (LDL) levels23 (Figure 1).
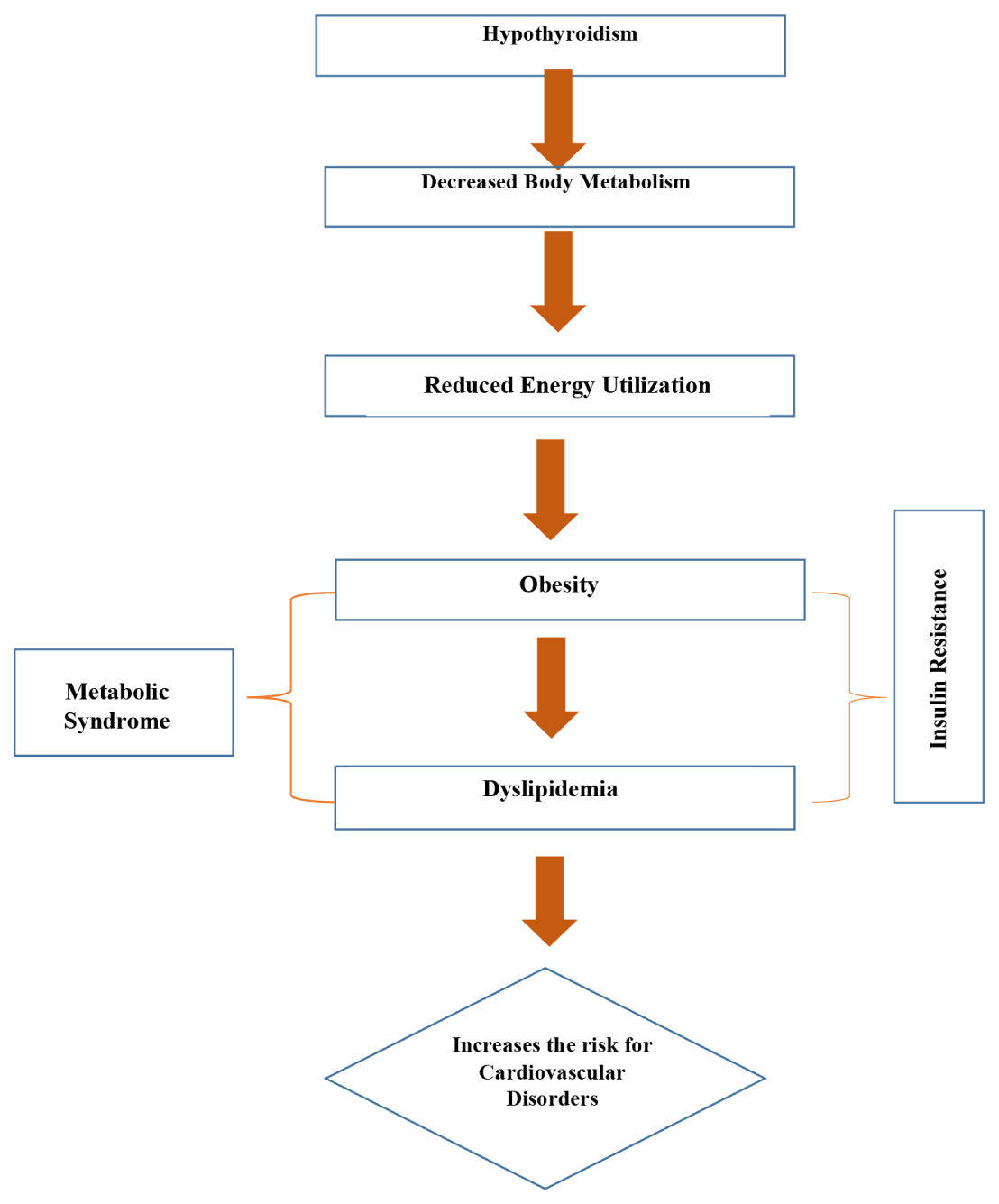
Figure 1.
Hypothyroidism with Metabolic syndrome leading to Cardiovascular Disorders.
Management of Metabolic Syndrome
Pharmacological Management of Metabolic Syndrome
According to the National Institutes of Health guidelines for the treatment of obesity, individuals with a BMI of at least 30 kg/m2 or those with a BMI of at least 27 kg/m2 with comorbidities related to their excess weight should seek pharmacological therapy for weight loss. Pharmacological management of weight loss includes treatment with appetite suppressants and inhibitors of nutrient absorption.24
Statins are an effective class of medications for lowering Low-Density Lipoprotein (LDL) levels, it has lesser drug interactions and side effects. Presently, there are seven different statins approved by the Food and Drug Administration (FDA), i.e., atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin. Researchers found that, when simvastatin was given at a dose of 20 mg or 40 mg to metabolic syndrome patients, LDL cholesterol decreased by 37.5% versus
36.0%, TG levels decreased by 24.1% versus 6.7%, and HDL cholesterol increased by 10.3% versus 0.6% when compared with the control group.25 The HMG-CoA reductase has a crucial role in the formation of cholesterol, cholesterol formation can be reduced by inhibiting the HMG-CoA reductase enzyme as a result of the number of Low-Density Lipoprotein receptors will increase, leading to a decrease in Low-Density Lipoprotein cholesterol levels.24
The metabolic abnormality should be treated simultaneously while treating hypertension also. Angiotensin-Converting Enzyme (ACE) inhibitors and Angiotensin Receptors Blockers (ARBs) are the medications of choice if not contraindicated. The use of Diuretics and calcium channel blockers (at low doses) seems to be effective. The Fixed-drug combinations of antihypertensive seem to be beneficial.26
Studies suggest that metformin,27 thiazolidinediones,28 and acarbose29 will reduce the risk of Type 2 Diabetes Mellitus in patients with impaired glucose tolerance. There was a subsequent reduction in metabolic syndrome in patients treated with metformin, the primary improvements were seen in weight control and fasting glucose. The use of Pioglitazone may be beneficial in high-risk patients with Type 2 Diabetes Mellitus to avoid cardiovascular events.30.
Non-Pharmacological Management of Metabolic Syndrome
Non-Pharmacologic management of metabolic syndrome includes dietary restrictions and increased physical activity. To avoid the risk of the metabolic syndrome they should avoid, high-calorie foods, red meats, sugars, and caffeinated drinks. Exercise has a major impact on metabolic syndrome. Moderate exercises like walking and weight training will be helpful to reduce the disease progression and cardiovascular complications.31
Thyroid Function and Cognitive Impairment
Cognitive domains can be affected by overt hypothyroidism. Studies reported that the cognitive domains like general intelligence, attention/ concentration, memory, perceptual function, language, psychomotor function, and executive functions will be affected due to clinical hypothyroidism. Thyroid Stimulating Hormone (TSH) can be correlated with cerebral function in mild cognitive impairment.30 Studies suggest that hypothyroidism was associated with progressive cognitive impairment and pseudodementia. Brain sensitivity to thyroid function variations was found to increase with age and variations in thyroid hormones. Proper treatment with hormone supplementation helps to prevent these symptoms and avoids other related complications.32
Cognitive Symptoms in Hypothyroidism
Cognitive impairments were not usually seen in subclinical hypothyroidism. But, In overt hypothyroidism, a wide range of cognitive domains were affected. Studies suggest that severe hypothyroidism can affect major domains of cognition like intelligence, attention, concentration, memory, psychomotor functions, executive functions, etc. Memory is the predominantly affected domain in cognition.33
The common cognitive symptoms exhibited by severe hypothyroidism patients were impaired consciousness, memory disturbances, and psychomotor slowing. In elderly patients, cognitive impairments can progress into dementia, if not treated. Improvements were seen in thyroid hormone supplementation therapy. But, cognitive impairments caused due to chronic thyroid hormone deficiency may not be reversible as always. It can even cause irreversible or permanent damage to the Central Nervous System (CNS).34
Thyroid Hormone Supplementation in Management of Cognitive Impairment
Treatment with Thyroid hormone supplementation therapy will help hypothyroid patients in relieve the symptoms, improving cognitive function associated with thyroid dysfunction, thereby reducing the neuropsychiatric symptoms, hospitalizations, and related expenses. It was observed that untreated hypothyroid patients showed some specific deficit in Memory retrieval, with more difficulty retrieving verbal information.35 Levothyroxine aids in the treatment of cognitive impairment caused by hypothyroidism.36
Levothyroxine Food and Drug Interactions
The food items such as soybean, papaya, grapefruit juice, and coffee can interact with Levothyroxine and reduce the oral absorption of levothyroxine.37 So, these food items should not be taken while taking levothyroxine tablets. It is advised to maintain at least two to four hours between the administration of levothyroxine and these foods. It is better to take levothyroxine early morning on an empty stomach. Levothyroxine can interact with proton pump inhibitors like lansoprazole and omeprazole and reduces the absorption of levothyroxine.37,38 Also,
the medicines such as calcium carbonate, calcium citrate, calcium acetate, aluminum hydroxide, cholestyramine, and ferrous sulphate can interact with levothyroxine and decrease the absorption of levothyroxine by binding to it, leading to the formation of complexes that are not absorbed. The absorption of levothyroxine can be decreased by interacting with sucralfate by interfering with its intra-luminal transport or by binding to it.38 The other medicines that interact with levothyroxine or thyroid hormones include anabolic steroids, androgens, beta-blockers, carbamazepine, cholestyramine, cimetidine, fluorouracil, glucocorticoids, heparin, lithium, phenobarbital, phenytoin, salicylates, and tolbutamide39,40 (Table 1).
| SL. No | Drug-Drug Interaction | Effect | Clinical Recommendations |
|---|---|---|---|
| 1 | Carvedilol45(Antihypertensive) | Carvedilol reduces the therapeutic efficacy of levothyroxine when used in combination. | Spacing between the medications is needed |
| 2 | Atorvastatin,46–48(Lipid-Lowering Agents) | Levothyroxine will decrease the metabolism of atorvastatin | Spacing between the medications is needed |
| 3 | Metformin49,50(Antidiabetic) | Levothyroxine reduces the therapeutic efficacy of metformin when used in combination | Monitoring of blood sugar levels is recommended |
| 4 | Aspirin51,52 (NSAIDs) | Levothyroxine increases the therapeutic efficacy of Aspirin | Monitor of INR level is needed |
Complications
Hypothyroidism can lead to many complications if not treated, the complications include, Myxedema coma, Cardiac diseases, Heart failure, Dyslipidemia, Mental retardation, Depression Infertility, Miscarriage, etc.41 So, proper treatment with thyroid hormone supplementation is important to get symptomatic relief, avoid disease progression and complications, and improve quality of life (Figure 2).
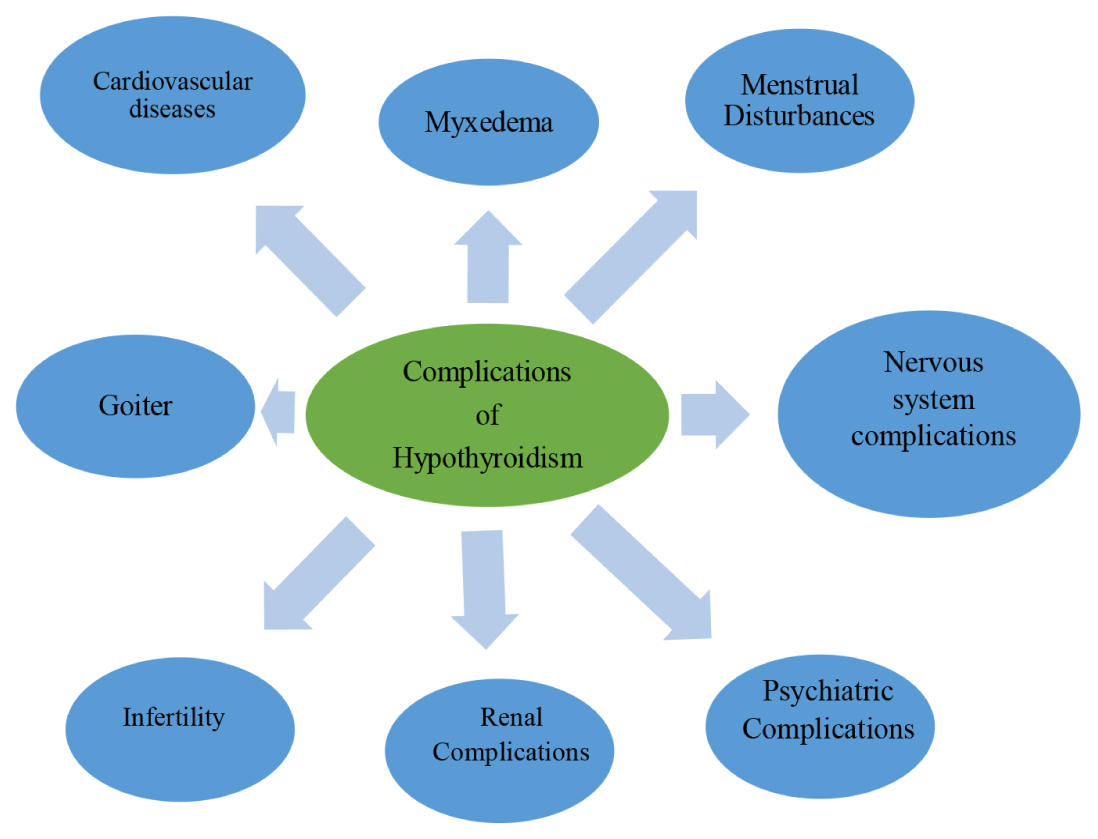
Figure 2.
Complications of Hypothyroidism
Quality of Life in Hypothyroidism
Studies suggested that the quality of life in hypothyroid patients can be impacted by many factors. Even though thyroid hormone supplementation provides symptomatic relief, the quality of life in hypothyroid patients can be enhanced by providing better patient-centered care with high-quality treatment and establishing a good rapport between the health care provider and the patient.42,43 Studies suggest that the quality of life of hypothyroid patients was not related to thyroid parameters. Increased body weight and Body Mass Index (BMI) was linked to a worse quality of life.44 Collaborative care provided by doctors, nurses, and pharmacists will enhance treatment quality and quality of life.
RECOMMENDATIONS
From the previously published literatures, it is evident that, in hypothyroid patients metabolic and cognitive symptoms are significant. It is necessary to provide pharmaceutical care to this population to improve the clinical outcomes and quality of life.
CONCLUSION
Hypothyroidism is a chronic condition with an underactive thyroid gland. It can lead to many complications if left untreated. Women are more at risk of hypothyroidism than men. Hypothyroidism exhibits a wide range of symptoms. As the symptoms of hypothyroidism are not specific, it is difficult to diagnose hypothyroidism based on its clinical presentation. A blood test, measuring the thyroid hormone levels, should be done to diagnose hypothyroidism. Cognitive symptoms associated with hypothyroidism are common in the elderly population. The cognitive dysfunctions may progress into dementia or may cause irreversible cerebral damage.
Patient counselling has an important role in hypothyroidism. Through patient education, the patient’s knowledge about their disease condition and medications can be improved. This makes them aware of the drug interactions and the direction of the use of the medicines. Through patient counselling, we can able to make the patients understand the importance of their therapy. Thereby, we can able to improve patient’s medication adherence and reduce medication-related problems and enhance the quality of life.
Cite this article
Shaji B, Joel JJ. Impact of Hypothyroidism on Metabolic and Cognitive Dysfunction: A Comprehensive Review. J Young Pharm. 2022;14(4):349-54.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
References
- Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550-62. [PubMed] | [CrossRef] | [Google Scholar]
- Uma D, Rabbani R, Lee JH, Gavini DR, Shah PH, Hamid P, et al. Does hormone supplementation with levothyroxine improve hypothyroid impaired cognitive dysfunction?. Cureus. 2021;13(9):e17885 [PubMed] | [CrossRef] | [Google Scholar]
- Almeida C, Vaisman M, Costa AJ, Reis FA, Reuters V, Teixeira P, et al. Are neuropsychological changes relevant in subclinical hypothyroidism?. Arq Bras Endocrinol Metabol. 2007;51(4):606-11. [PubMed] | [CrossRef] | [Google Scholar]
- Duntas LH, Jonklaas J. Levothyroxine dose adjustment to optimise therapy throughout a patient’s lifetime. Adv Ther. 2019;36(Suppl 2):30-46. [PubMed] | [CrossRef] | [Google Scholar]
- Mullur R, Liu YY, Brent GA. Thyroid hormone regulation of metabolism. Physiol Rev. 2014;94(2):355-82. [PubMed] | [CrossRef] | [Google Scholar]
- Gaitonde DY, Rowley KD, Sweeney LB. Hypothyroidism: an update. Am Fam Physician. 2012;86(3):244-51. [PubMed] | [CrossRef] | [Google Scholar]
- Persani L. Clinical review: Central hypothyroidism: pathogenic, diagnostic, and therapeutic challenges. J Clin Endocrinol Metab. 2012;97(9):3068-78. [PubMed] | [CrossRef] | [Google Scholar]
- Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489-99. [PubMed] | [CrossRef] | [Google Scholar]
- Hoogendoorn EH, Hermus AR, de Vegt F, Ross HA, Verbeek AL, Kiemeney LA, et al. Thyroid function and prevalence of anti-thyroperoxidase antibodies in a population with borderline sufficient iodine intake: influences of age and sex. Clin Chem. 2006;52(1):104-11. [PubMed] | [CrossRef] | [Google Scholar]
- Nagendiran A, Kalaimani K, Anantharani K. Assessment of knowledge, practice and treatment adherence of patients with hypothyroidism in endocrinology department. Int J Nutr Pharmacol Neurol Dis. 2021;11:189-93. [PubMed] | [CrossRef] | [Google Scholar]
- Yadav V, Dabar D, Goel AD, Bairwa M, Sood A, Prasad P, et al. Prevalence of hypothyroidism in pregnant women in India: A meta-analysis of observational studies. J Thyroid Res. 2021;2021:5515831 [PubMed] | [CrossRef] | [Google Scholar]
- Chiovato L, Magri F, Carlé A. Hypothyroidism in context: where we’ve been and where we’re going. Adv Ther. 2019;36(Suppl 2):47-58. [PubMed] | [CrossRef] | [Google Scholar]
- Rochlani Y, Pothineni NV, Kovelamudi S, Mehta JL. Metabolic syndrome: pathophysiology, management, and modulation by natural compounds. Ther Adv Cardiovasc Dis. 2017;11(8):215-25. [PubMed] | [CrossRef] | [Google Scholar]
- Magri F, Chiovato L, Croce L, Rotondi M. Thyroid hormone therapy for subclinical hypothyroidism. Endocrine. 2019;66(1):27-34. [PubMed] | [CrossRef] | [Google Scholar]
- Bensenor IM, Olmos RD, Lotufo PA. Hypothyroidism in the elderly: diagnosis and management. Clin Interv Aging. 2012;7:97-111. [PubMed] | [CrossRef] | [Google Scholar]
- Clyde PW, Harari AE, Getka EJ, Shakir KM. Combined levothyroxine plus liothyronine compared with levothyroxine alone in primary hypothyroidism: a randomized controlled trial. JAMA. 2003;290(22):2952-8. [PubMed] | [CrossRef] | [Google Scholar]
- Walsh JP, Shiels L, Lim EM, Bhagat CI, Ward LC, Stuckey BG, et al. Combined thyroxine/liothyronine treatment does not improve well-being, quality of life, or cognitive function compared to thyroxine alone: a randomized controlled trial in patients with primary hypothyroidism. J Clin Endocrinol Metab. 2003;88(10):4543-50. [PubMed] | [CrossRef] | [Google Scholar]
- Sahay RK, Nagesh VS. Hypothyroidism in pregnancy. Indian J Endocrinol Metab. 2012;16(3):364-70. [PubMed] | [CrossRef] | [Google Scholar]
- Chopra IJ, Baber K. Treatment of primary hypothyroidism during pregnancy: is there an increase in thyroxine dose requirement in pregnancy?. Metabolism. 2003;52(1):122-8. [PubMed] | [CrossRef] | [Google Scholar]
- Werneck FZ, Coelho EF, Almas SP, Garcia MMDN, Bonfante HLM, Lima JRP, et al. Exercise training improves quality of life in women with subclinical hypothyroidism: a randomized clinical trial. Arch Endocrinol Metab. 2018;62(5):530-6. [PubMed] | [CrossRef] | [Google Scholar]
- Bansal A, Kaushik A, Singh CM, Sharma V, Singh H. The effect of regular physical exercise on the thyroid function of treated hypothyroid patients: an interventional study at a tertiary care center in Bastar region of India. Arch Med Health Sci. 2015;3(2):244 [CrossRef] | [Google Scholar]
- Sharma R, Bharti S, Kumar KH. Diet and thyroid-myths and facts. J Med Nutr Nutraceuticals. 2014;3(2):60 [CrossRef] | [Google Scholar]
- Grundy SM, Hansen B, Smith SC, Cleeman JI, Kahn RA. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation, Conference Participants. 2004;109(4):551-6. CIR.0000112379.88385.67 [PubMed] | [CrossRef] | [Google Scholar]
- Binesh Marvasti TB, Adeli Kh. Pharmacological management of metabolic syndrome and its lipid complications. Daru. 2010;18(3):146-54. [PubMed] | [Google Scholar]
- Lundbye JB, Thompson PD. Statin use in the metabolic syndrome. Curr Atheroscler Rep. 2005;7(1):17-21. [PubMed] | [CrossRef] | [Google Scholar]
- Israili ZH, Lyoussi B, Hernández-Hernández R, Velasco M. Metabolic syndrome: treatment of hypertensive patients. Am J Ther. 2007;14(4):386-402. [PubMed] | [CrossRef] | [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403. [PubMed] | [CrossRef] | [Google Scholar]
- Knowler WC, Hamman RF, Edelstein SL, Barrett-Connor E, Ehrmann DA, Walker EA, et al. Prevention of type 2 diabetes with troglitazone in the Diabetes Prevention Program. Diabetes. 2005;54(4):1150-6. [PubMed] | [CrossRef] | [Google Scholar]
- Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359(9323):2072-7. [PubMed] | [CrossRef] | [Google Scholar]
- Rajagopalan R, Iyer S, Khan M. Effect of pioglitazone on metabolic syndrome risk factors: results of double-blind, multicenter, randomized clinical trials. Curr Med Res Opin. 2005;21(1):163-72. [PubMed] | [CrossRef] | [Google Scholar]
- Wirth A. Non-pharmacological therapy of metabolic syndrome. Herz. 1995;20(1):56-69. [PubMed] | [Google Scholar]
- Beydoun MA, Beydoun HA, Kitner-Triolo MH, Kaufman JS, Evans MK, Zonderman AB, et al. Thyroid hormones are associated with cognitive function: moderation by sex, race, and depressive symptoms. J Clin Endocrinol Metab. 2013;98(8):3470-81. [PubMed] | [CrossRef] | [Google Scholar]
- Samuels MH. Psychiatric and cognitive manifestations of hypothyroidism. Curr Opin Endocrinol Diabetes Obes. 2014;21(5):377-83. [PubMed] | [CrossRef] | [Google Scholar]
- Nomoto S, Kinno R, Ochiai H, Kubota S, Mori Y, Futamura A, et al. The relationship between thyroid function and cerebral blood flow in mild cognitive impairment and Alzheimer’s disease. PLOS ONE. 2019;14(4):e0214676 [PubMed] | [CrossRef] | [Google Scholar]
- Miller KJ, Parsons TD, Whybrow PC, van Herle K, Rasgon N, van Herle A, et al. Memory improvement with treatment of hypothyroidism. Int J Neurosci. 2006;116(8):895-906. [PubMed] | [CrossRef] | [Google Scholar]
- Khaleghzadeh-Ahangar H, Talebi A, Mohseni-Moghaddam P. Thyroid disorders and development of cognitive impairment: a review study. Neuroendocrinology. 2022;112(9):835-44. [PubMed] | [CrossRef] | [Google Scholar]
- Colucci P, Yue CS, Ducharme M, Benvenga S. A review of the pharmacokinetics of levothyroxine for the treatment of hypothyroidism. Eur Endocrinol. 2013;9(1):40-7. [PubMed] | [CrossRef] | [Google Scholar]
- Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave GD, et al. Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006;354(17):1787-95. [PubMed] | [CrossRef] | [Google Scholar]
- Sachmechi I, Reich DM, Aninyei M, Wibowo F, Gupta G, Kim PJ, et al. Effect of proton pump inhibitors on serum thyroid-stimulating hormone level in euthyroid patients treated with levothyroxine for hypothyroidism. Endocr Pract. 2007;13(4):345-9. [PubMed] | [CrossRef] | [Google Scholar]
- Liwanpo L, Hershman JM. Conditions and drugs interfering with thyroxine absorption. Best Pract Res Clin Endocrinol Metab. 2009;23(6):781-92. [PubMed] | [CrossRef] | [Google Scholar]
- Abid M, Sharma KK, Ali SS, Chandra P, Verma A, Kishore K, et al. Complication and management of hypothyroidism: a review. Indian J Drugs. 2016;4(2):42-56. [PubMed] | [CrossRef] | [Google Scholar]
- Shivaprasad C, Rakesh B, Anish K, Annie P, Amit G, Dwarakanath CS, et al. Impairment of health-related quality of life among Indian patients with hypothyroidism. Indian J Endocrinol Metab. 2018;22(3):335-8. [PubMed] | [CrossRef] | [Google Scholar]
- Mitchell AL, Hegedüs L, Žarkovic M, Hickey JL, Perros P. Patient satisfaction and quality of life in hypothyroidism: an online survey by the British Thyroid Foundation. Clin Endocrinol (Oxf). 2021;94(3):513-20. [PubMed] | [CrossRef] | [Google Scholar]
- Kelderman-Bolk N, Visser TJ, Tijssen JP, Berghout A. Array. Eur J Endocrinol. 2015;173(4):507-15. [PubMed] | [CrossRef] | [Google Scholar]
- Wiersinga WM. Propranolol and thyroid hormone metabolism. Thyroid. 1991;1(3):273-7. [PubMed] | [CrossRef] | [Google Scholar]
- Backman JT, Filppula AM, Niemi M, Neuvonen PJ. Role of cytochrome P450 2C8 in drug metabolism and interactions. Pharmacol Rev. 2016;68(1):168-241. [PubMed] | [CrossRef] | [Google Scholar]
- Totah RA, Rettie AE. Cytochrome P450 2C8: substrates, inhibitors, pharmacogenetics, and clinical relevance. Clin Pharmacol Ther. 2005;77(5):341-52. [PubMed] | [CrossRef] | [Google Scholar]
- Daily EB, Aquilante CL. Cytochrome P450 2C8 pharmacogenetics: a review of clinical studies. Pharmacogenomics. 2009;10(9):1489-510. [PubMed] | [CrossRef] | [Google Scholar]
- Sandler MP, Robinson RP, Rabin D, Lacy WW, Abumrad NN. The effect of thyroid hormones on gluconeogenesis and forearm metabolism in man. J Clin Endocrinol Metab. 1983;56(3):479-85. [PubMed] | [CrossRef] | [Google Scholar]
- McCulloch AJ, Johnston DG, Baylis PH, Kendall‐Taylor P, Clark F, Young ET, et al. Evidence that thyroid hormones regulate gluconeogenesis from glycerol in man. Clin Endocrinol (Oxf). 1983;19(1):67-76. [PubMed] | [CrossRef] | [Google Scholar]
- Wang R, Nelson JC, Wilcox RB. Salsalate and salicylate binding to and their displacement of thyroxine from thyroxine-binding globulin, transthyrin, and albumin. Thyroid. 1999;9(4):359-64. [PubMed] | [CrossRef] | [Google Scholar]
- Larsen PR. Salicylate-induced increases in free triiodothyronine in human serum. Evidence of inhibition of triiodothyronine binding to thyroxine-binding globulin and thyroxine-binding prealbumin. J Clin Invest. 1972;51(5):1125-34. [PubMed] | [CrossRef] | [Google Scholar]
