ABSTRACT
The Severe Acute Respiratory Syndrome (SARS-CoV-2) pandemic has reverberated into calamitous illness globally, even though children have been comparatively reprieved. Coronavirus-associated multisystem inflammatory syndrome (MIS) has been outlined in children (MIS-C) and hardly ever in adults (MIS-A) in as much as April and June 2020, sequentially. Whilst the rudimentary immunopathology is not well demarcated, adaptive immunity is contemplated to be blameworthy. We report a case of Multisystem inflammatory syndrome in children lie illness – MIS-A who presented with fever, pain abdomen, weakness and low oxygen saturation in an emergency. Truenat for SARS-CoV-2 came out negative but covid serology IGG came positive. The clinical presentation of the patient was in maintained with the clinically accepted definition of MIS-A.
INTRODUCTION
The Severe Acute Respiratory Syndrome (SARS-CoV-2) infection has reverberated into calamitous illness globally thus declared as a pandemic, even though children have been comparatively reprieved.Scathing lung inclusion in addition with acute respiratory failure is the most frequent impediment of ongoing pandemic in adults, but many have multiple organs complication, including the heart.1 Coronavirus-associated multisystem inflammatory syndrome (MIS) has been outlined in children (MIS-C) and hardly ever in adults (MIS-A) in as much as April and June 2020, sequentially. The fever is the dominant detection of the syndrome with preponderant detections in major organ systems like gastrointestinal, cardiovascular, haematological, and dermatological. MIS should be held back in intellect the patient with neoteric coronavirus infectivity, conferring outcomes and lab peculiarities recommending hyperinflation (like elevation of ferritin levels, increase in C-reactive protein (CRP), prominent lymphocytopenia).2
CASE REPORT
A 21-year-old female came to emergency with no consequential past history having chief complaints of pyrexia for 4 days which was high grade (fever to 104°F) not associated with chill and rigor. Patient also complaints of diffuse abdominal pain for 2 days, associated with nausea, vomiting and generalized weakness. No history of any chest pain, shortness of breath, palpitation, swelling, headache, seizures. At admission, patient was conscious, oriented, following commands, recorded fever stands at 101°F, cardiac rate stands at 138 beats per minute, with respiratory breath stands at 24 breaths, hypotensive with blood pressure was 60/40 mmHg requiring conglomerate fluid boluses and inotrope as noradrenaline and oxygen saturation was 84% on room air thus was kept on 4L of oxygen with simple face mask where saturation was maintained at 96%. On respiratory examination, there was reduced bilateral air entry with crepitations over lower zone. Per abdomen soft, non-tender. Neurological examination was well within normal limit. Cardiovascular examination was normal, S1S2 heard, no murmur present, JVP was under normal range. Her Chest X-ray was done which was s/o bilateral blunting of cardio phrenic angle – bilateral pleural effusion with bilateral lower zone air space infiltration suggestive of B/L lower lobe pneumonitis (Figure 1, 2). Her routine investigations were sent with fever panel which came negative. At same time, her TrueNAT for SARS-CoV-2 came out to be negative. On investigations the patient was found to be lymphopenic, with decreased platelet count, low albumin levels, elevated inflammatory markers, D-dimer, and CRP as shown in Table1. Antibody test with IgG was positive.
| Age | 21 years |
| Sex | Female |
| BMI | |
| Co- morbidities | None |
| Maximum body temperature | 103 (F) |
| Evidence of clinically severe illness requiring hospitalization, with multisystem (>2) organ involvement | |
| Cardiac (e.g., shock, elevated troponin, BNP, abnormal echocardiogram, arrhythmia) | Yes |
| Renal (e.g., acute kidney injury or renal failure) | Yes |
| Hematological (e.g., elevated D-dimers, thrombophilia, or thrombocytopenia) | Yes |
| Gastrointestinal (e.g., elevated bilirubin, elevated liver enzymes, or diarrhea) | Yes |
| Dermatological (e.g., rash, mucocutaneous lesions) | No |
| Neurological (e.g., CVA, aseptic meningitis, encephalopathy) | No |
| COVID-19 exposure within the 4 weeks prior to the onset of MIS-A symptoms | No |
| RT-PCR | Negative |
| SARS-CoV-2 total antibody | Positive |
| WBC | 4.74/cumm |
| PLATELETS | 65/cumm |
| CRP | 226 mg/l |
| D-DIMER | 1193 ng/ml |
| ESR | 110 mm1st hour |
| CREATININE | 1.79 mg/dl |
| LDH | 176 IU/L |
| ALBUMIN | 2.3 gm/dl |
The patient was managed with broad-spectrum parenteral antibiotics (meropenem and clindamycin), I.V Steroids (methylprednisolone) and s/c Anticoagulant (enoxaparin). However, due to congestion in lungs and higher oxygen requirements, she was kept on Non-invasive ventilation with fio2 90%. inspite of NIV she was not maintaining saturation and developed pulmonary failure thus the endotracheal tube was inserted and patient was shifted to mechanical ventilator. She was extubated on day 6th of hospitalization and was kept on high flow 12-15 liter of oxygen with venturi mask and maintained saturation of around 92-94%. Progressive chest radiographs on day 5 and day 11 showed improvement and reduction in ground glass opacities. She was shifted to ward and started with I.V ceftriaxone and tab methylprednisolone along with other supportive treatment. She was kept on oxygen support via venturi face mask. She was maintaining 96% saturation at 5L/min oxygen. Her condition improved gradually over course of stay. Her oxygen requirement gradually decreased. Dose of steroids were tapered off. On 12th day, she was maintaining 97% oxygen saturation on room air. Patient was discharged on 14th day with normal vitals and maintaining 98% Spo2 on room air. The clinical presentation of the patient was in maintained with the clinically accepted definition of MIS-A. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
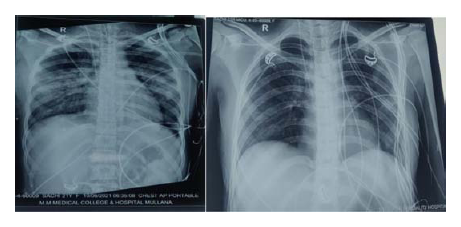
Figure 1.
Chest Radiographs on Day 1 and Day 3 respectively.
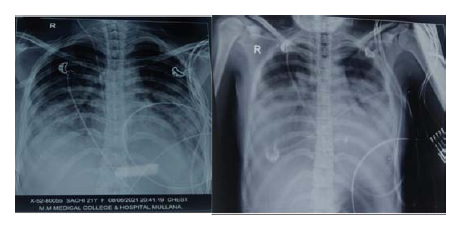
Figure 2.
Chest Radiographs on Day 5 and Day 11 respectively.
DISCUSSION
MIS-C is a hyper-inflammatory syndrome that strikes multiple organs and is provoked by SARS-CoV-2 infection. This inflammatory disease is contemplated as a post SARS-CoV-2 complication relatively than an infectious disease in astute development state.3 Though there is some manifoldness of manifestations and findings, the gastrointestinal manifestations like pain in the abdomen, vomiting, myocarditis, diarrhea, fever, hypotension, and shock are the prominent ones.
CONCLUSION
Coronavirus-associated MIS has been outlined in children (MIS-C) and minimever in adults (MIS-A).
Cite this article
Batra N, Kaur N. Multisystem Inflammatory Syndrome in Adults (MIS-A): A Case Report. J Young Pharm. 2022;14(4):449-50.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
References
- Feldstein L R, Rose E B. Array. 2020;383(4):334-46.
- Kabeerdoss J, Pilania R K. “Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: Immunological mechanisms, clinical manifestations and management.”. Rheumatology International. 2021;41(1):19-32. [Google Scholar]
- Morris SB, Schwartz NG, Patel P, Abbo L, Beauchamps L, Balan S, Lee EH, Paneth-Pollak R, Geevarughese A, Lash MK, et al. Case series of multisystem inflammatory syndrome in adults associated with SARS-CoV-2 infection— United Kingdom and United States. 2020 [Google Scholar]
