ABSTRACT
Anabolic androgenic steroids are a type of synthetic testosterone which are most likely used by athletes, body builders and physicians to increase male sex hormones in those who have not yet reached puberty. We present the case of 32-years-old male patient who was admitted in respiratory ward with complaints of breathlessness and weakness. Patient had history of left hydropneumothorax secondary due to pulmonary tuberculosis, iatrogenic cushing syndrome and was misusing anabolic androgenic steroids for muscle gain for a long time. The laboratory investigations were noted that elevation of liver function tests, abnormal haematological tests, ultrasonography was revealed to be hepatomegaly with grade II fatty liver. The patient was treated with the Dexamethasone, combination of Piperacillin and Tazobactam, combination of Metadoxine, Silymarin and l-Ornithinel-Aspartate (LOLA), Clonazepam, Ketoconazole and his health condition improved enough for him to be discharged. In conclusion we recommend the health care professionals to review the safety profile, examine laboratory results and counsel patients to prevent further abusage of anabolic androgenic steroids.
INTRODUCTION
Anabolic Androgenic Steroids (AAS) are testosterone-derived compounds that act on testosterone receptors for efficiently increasing muscle mass, improving physical appearance by stimulating protein synthesis through a physiological rise in testosterone hormone.1 These steroids are widely used from medical emergencies to misuse by athletes.2 US FDA has approved use of AAS primarily for the treatment of male hypogonadism, wasting syndrome in HIV infection and anemia.3 Unfortunately, it is frequently misused in spite of its rational use due to easily accessible being available as Over The Counter (OTC).4 On prolonged misuse of AAS leads to life threatening conditions and adverse effects ranging from mild hepatitis to cardiac death.5 Furthermore, the severity of adverse effects depends on duration and dose of drug abuse. According to recent study revealed that 1% of general population is on systemic glucocorticosteroids for the year 2011.6 However, abuse of steroids is less infrequent in Asian countries due to lack of cultural prominence on muscularity. Here we report a rare case of Indian male patient who misused AAS medications for a long time, resulting in immune system deterioration, Anti-tubercular therapy (ATT) induced hepatitis and iatrogenic cushing’s syndrome.
CASE SUMMARY
A 32-years-old male patient was hospitalized to the department of pulmonary medicine with complaints of breathlessness for five days and generalized weakness for one week. On admission his previous records shown that he was admitted in view of left hydropneumothorax secondary to pulmonary tuberculosis and on medication of antitubercular with combination of Tablets Rifampicin, Isoniazid, Pyrazinamide, Ethambutol (four tablets daily in the morning 30 min before food or 2 hr after the food). He was also diabetic for a year and is currently on Metformin 500 mg twice daily (BD). Patient was a professional gym trainer who was misusing unknown anabolic steroids, a synthetic of testosterone for muscle gain. There was no history of allergy was reported by the patient or found in his previous medical records. On general examination he was found to be conscious, oriented, systemic examination revealed tachycardia, Per Abdomen (PA) was soft mild tenderness in Residual Vector Quantization (RVQ).
The laboratory investigations revealed that liver functions tests are elevated i.e. total bilirubin 3.83 mg/dL (0.00-1.40 mg/dL), direct bilirubin 3.8mg/dL (0.00-0.30), total protein 4.2g/ dL (6.6-8.7 g/dL), Serum Glutamic-Oxaloacetic Transaminase (SGOT) 139 U/L (1-40 U/L), Serum Glutamic Pyruvic Transaminase (SGPT) 67 U/L (1.-41 U/L), Alkaline Phosphatase (ALP) 197 U/L (40-130 U/L). Haematological test haemoglobin level was 9.1 mg/dL, White Blood Cells (WBC) were 9.5 cells/ cumm, Neutrophils 68, leucocytes 19 and platelet count 3.64 lakh/ cmm. Ultrasound of pelvis and abdomen showed hepatomegaly (16.5 cm) with grade II fatty liver, inflammatory (hepatitis) etiology and mild splenomegaly and minimal left pleural effusion (Figure 1). Anti-tubercular therapy induced hepatitis was detected after consulting a gastroenterologist. A psychiatry referral was also obtained, and dissociative /attention seeking disorder was identified.
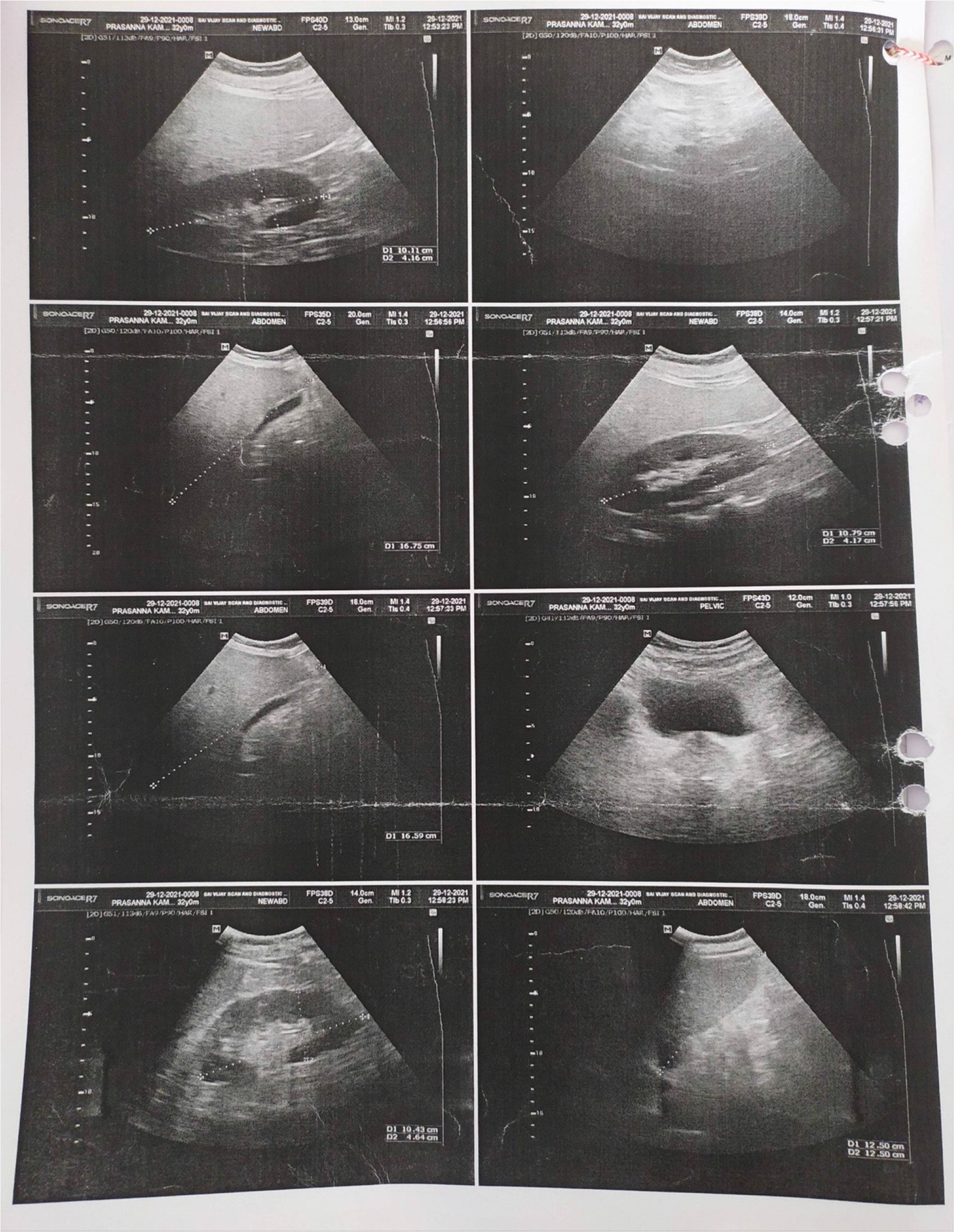
Figure 1:
Hepatomegaly (16.5 cm) with grade II fatty liver, inflammatory (hepatitis) etiology and mild splenomegaly and minimal left pleural effusion.
The patient was diagnosed with iatrogenic cushing syndrome based on clinical signs and previous medical history, and was treated with Tablet. Ketoconazole 200mg BD BD for iatrogenic cushing syndrome. The patient was eventually discovered to be misusing anabolic steroids (testosterone) injections for muscle growth which led to iatrogenic cushing syndrome. However, the Tablet Dexamethasone 2mg BD was continued for the patient. During the hospital stay, the patient was given Injection Piperacillin and Tazobactam 4.5gm Intravenous (IV) four times a day (QID) days, Tablet Metformin 500mg BD, Tablet Ursodeoxycholic acid 300mg three times a day (TID), Tablet Pantoprazole 40mg BD, Capsule vitamin B-complex with Vitamin C Once Daily (OD), Syrup Ambroxol hydrochloric acid, Terbutaline sulphate and Guaiphenesin 10mL three TID for 5 days, Tablet Ademetionine 400mg BD for 5 days, Tablet vitamin E 400mg OD for 5 days, Tablet Metadoxine, Silymarin and LOLA BD for 5 days, Tablet Clonazepam 0.5mg OD for 5 days, Tablet Ketoconazole 200mg BD for 5 days. The patient remained stable and his condition improved during the course of the hospital stay. After a week of hospitalization patient was discharged and advised to not to take any steroids in future.
DISCUSSION
Anabolic androgenic steroids are synthetic or man-made available testosterone. The testosterone is the common sexual hormone found in the men more compared to women. Men’s sexual features such as deep voice, facial hair, and muscle growth are maintained by the testosterone hormone. These anabolic steroids are used by bodybuilders and athletes to build muscles and increse athletic performance. This type of anabolic steroid abuse causes acne, slowed growth in teenagers, high blood pressure, heart difficulties, liver and kidney damage, baldness, infertility, etc.7 In our study we found similar instance with the patient who misused these anabolic steroids for body muscle growth.
The most common self-report untoward effects of short or long-term AAS abuse of male athletes usually reports an increase in sexual drive, acne vulgaris, increased body hair and increase in aggressive behaviour. Increased blood pressure, disturbances in endocrine and immunological function, changes in the sebaceous system and skin, and changes in the haemostatic system and urogenital tract are among the other side effects.8 A study showed a gallop rhythm and an apical pan systolic murmur in a patient who misused steroids.9 Similarly in our case patient had tachycardia. Liver functions tests such as total bilirubin, direct bilirubin, Total protein, SGOT, SGPT, Alkaline phosphatase were found be elevated similar to another study in which a 26-year-old male patient who had misused anabolic drugs developed clinical jaundice, elevated bilirubin levels, Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), Alkaline Phosphatase (ALP).10 Our patient was diagnosed with dissociative /attention seeking illness, according to the psychiatry reference. In another study, anabolic-androgenic steroids were found to both treat and cause depression. Depression may occur as a result of anabolic-androgenic steroid withdrawal or reduced use.11 Prolong use of AAS and intake of prescribed antitubercular drugs in our patient resulted in hepatomegaly and hepatitis, a scenario that has been documented in previous study where AAS has damaged the liver and caused liver toxicity.12 Previous history of anabolic steroids (testosterone) injections and Tablet Dexamethasone use in our patient resulted in iatrogenic cushing syndrome, as documented in a comparable earlier investigation. Prolonged use of AAS resulted in iatrogenic cushing syndrome.13 In our patient, the Naranjo causality assessment score was found to be 4, indicating that a possible reaction of AAS misuse.14 Other severity of AAS induced iatrogenic cushing syndrome was assessed by using Modified Hartwig and Siegel scale and the severity was determined to be at level 3.15 The physician reduced the amount of dexamethasone to 0.5 mg every 6 hr (9 AM, 3 PM, 9 PM, 3 AM) for two days, according to the low dose dexamethasone suppression test (DST), in order to prevent further damage to the patient’s liver, immune system, and other organs.16
CONCLUSION
This case demonstrates an evidence of lack of awareness among patients or steroid users about the rational use of steroids, which has resulted in catastrophic health consequences. We advise the physicians, nurses and pharmacists to pay greater attention to review and collect the past medication history, laboratory parameters, psychological behaviour on regular basis, and to counsel patients about rational use of medications in order to prevent misuse of drugs. Furthermore, raising awareness, training, and educating people about AAS usage will help to reduce the severity of AAS-related problems.
References
- Franey DG, Espiridion ED. Anabolic steroid-induced mania. Cureus. 2018;10(8):e3163 [PubMed] | [CrossRef] | [Google Scholar]
- Samreen F, Popal U, Baloch ZA. Anabolic steroid-induced myocardial infarction in a young male. Cureus. 2021;13(2):1-4. [PubMed] | [CrossRef] | [Google Scholar]
- Garner O, Iardino A, Ramirez A, Yakoby M. Cardiomyopathy induced by anabolic-androgenic steroid abuse. B.M.J. Case Rep.. 2018;2018:bcr-2017 [PubMed] | [CrossRef] | [Google Scholar]
- Luc JG, Buchholz H, Kim DH, MacArthur RG. Left ventricular assist device for ventricular recovery of anabolic steroid-induced cardiomyopathy. J Surg Case Rep. 2018;2018(8):1-3. [PubMed] | [CrossRef] | [Google Scholar]
- Hernández-Guerra AI, Tapia J, Menéndez-Quintanal LM, Lucena JS. Sudden cardiac death in anabolic androgenic steroids abuse: case report and literature review. Forensic Sci Res. 2019;4(3):267-73. [PubMed] | [CrossRef] | [Google Scholar]
- Rajan R, Kuriakose C, Paul J, Kapoor N, Cherian KE, Paul TV, et al. A rare cause of familial exogenous Cushing syndrome. J Fam Med Prim Care. 2019;8(5):1798-800. [PubMed] | [CrossRef] | [Google Scholar]
- Hoffman JR, Ratamess NA. Medical issues associated with anabolic steroid use: are they exaggerated?. J Sports Sci Med.. 2006;5(2):182-93. [PubMed] | [Google Scholar]
- Hartgens F, Kuipers H. Effects of androgenic-Anabolic Steroids in athletes. Sports Med. 2004;34(8):513-54. [PubMed] | [CrossRef] | [Google Scholar]
- Vanberg P, Atar D. Androgenic anabolic steroid abuse and the cardiovascular system. Handb Exp Pharmacol. 2010;19(195):411-57. [PubMed] | [CrossRef] | [Google Scholar]
- Stimac D, Milić S, Dintinjana RD, Kovac D, Ristić S. Androgenic/anabolic steroid-induced toxic hepatitis. J Clin Gastroenterol.. 2002;35(4):350-2. [PubMed] | [CrossRef] | [Google Scholar]
- Uzych L. Anabolic-androgenic steroids and psychiatric-related effects: a review. Can J Psychiatry Rev Canadienne Psychiatr. 1992;37(1):23-8. [PubMed] | [CrossRef] | [Google Scholar]
- Sánchez-Osorio M, Duarte-Rojo A, Martínez-Benítez B, Torre A, Uribe M. Anabolic androgenic steroids and liver injury. Liver Int. 2008;28(2):278-82. [PubMed] | [CrossRef] | [Google Scholar]
- Nizar H, Aylwin S. A case of iatrogenic Cushing. Endocr Admin.. 2017;48 [PubMed] | [CrossRef] | [Google Scholar]
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-45. [PubMed] | [CrossRef] | [Google Scholar]
- S P, K M, S A. Causality, severity and preventability assessment of adverse cutaneous drug reaction: a prospective observational study in a tertiary care hospital. J Clin Diagn Res. 2013;7(12):2765-7. [PubMed] | [CrossRef] | [Google Scholar]
- Dogra P, Vijayashankar NP. Dexamethasone suppression test. StatPearls. 2022 [PubMed] | [CrossRef] | [Google Scholar]
