ABSTRACT
Background
The standard treatment of type II diabetes mellitus (T2DM) more often explicitly decreased efficacy resulting in improper glycemic control. Hence, there is a need for alternative therapy like Gliptins, which play a key role in the management of diabetes mellitus. The current research studies the prescription pattern analysis of Teneligliptin in the therapy of T2DM patients.
Materials and Methods
The investigation was a prospective observational study with a sample size of 302 cases in a diabetic centre in Erode, India. The patients were prescribed Teneligliptin along with Insulin and other oral antidiabetic drugs (OAD) and drugs for other co-morbid conditions. Patient details were collected in connection to prescribed medicines, biochemical lab data, other co-morbid conditions, and complications related to T2DM.
Results
The prescription patterns of about 302 patients with T2DM, initially prescribed with gliptin, were reviewed. Teneligliptin was the gliptin drug prescribed along with insulin and other OADs. The commonly prescribed regimen was a combination of Teneligliptin, Metformin and Glibenclamide. Out of 302 patients, 169 were men and 133 were women within the age category of 50-59 years. The result of this study shows that the duration of diabetes and gender was statistically significant with p-value < 0.003 and 0.01 respectively.
Conclusion
The analysis disclosed that the most repeatedly prescribed DPP4 inhibitor is Teneligliptin, mostly prescribed as an add-on therapy with metformin, insulin and other OAD drugs. Also, the current drug treatment and the planning of multiple drug interventions with changes in lifestyle for T2DM are much needed.
INTRODUCTION
Diabetes mellitus (DM), a heterogeneous complex metabolic disorder, characterized by elevated blood glucose concentrations due to resistance towards the action of insulin, and/or insufficient insulin secretion. Type II DM (T2DM) is an endocrine, metabolic disorder marked by an increased blood sugar level (hyperglycemia). T2DM is a global disease that has been affected all over the world.1 Presently, 62.4 million people have T2DM in India. It is expected to increase to over 100 million by 2030. T2DM is a main cause of morbidity and death in all ages and is accordingly a significant health issue.2
Approximately 90% of T2DM cases are described by the presence of both insulin resistance and relative insulin deficit. Insulin resistance is alleviated by increasing the breakdown of lipids and free fatty acid production, including decreased accumulation of muscle tissue glucose.3 Beta-cell disorder worsens over time leading to impaired blood sugar tolerance. T2DM arises when a diabetogenic lifestyle (excess calorie, insufficient physical activity and fatness) and a susceptible phenotype is linked.4
Insulin and oral antidiabetic drugs (OADs) are not the only therapeutic treatments for T2DM that provide a targeted level of health, the rational use of insulin and OADs are also essential for the efficacy and adequate therapeutic interventions.5,6 DPP-4 inhibitors (DPP-4i) enhance glucose sensitivity of α and β cells, promote insulin and lowers Glucagon release, such as glucagon-like peptide-1and Glucose-dependent insulinotropic peptide.4 Teneligliptin and sitagliptin, gliptins of the third generation, are inhibitors of class 3 and teneligliptin is five times more active than sitagliptin. Its distinct J-shaped structure of 5 successive rings (Figure 1) gives a potent and long-lasting action. Furthermore, it has a distinct structure and attaches to the S1, S2, & S2 extensive sub-sites of the DPP-4i enzyme, resulting in increased potency and selectivity. Clinically, teneligliptin can be prescribed in once-daily dosing and possesses DPP-4 maximum inhibition within 2h, 24-h glycaemic control, minimum pharmaceutical drug-drug interaction, and good hepatic clearance.7–8
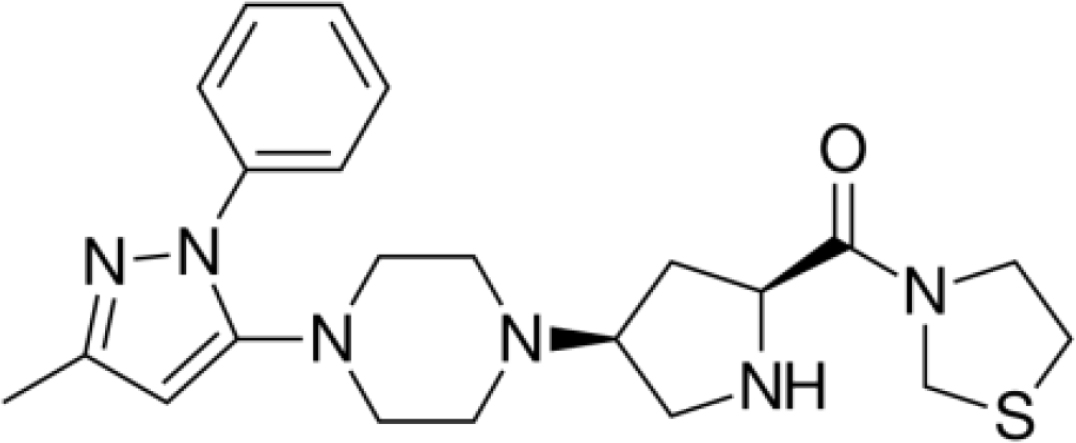
Figure 1:
Structure of Teneligliptin.
Rational drug utilization means that a person gets the right medicine at the right time, in the right quantity, for the right duration, with the right information and follow-up treatment, and at a good price.9 Prescription pattern analysis is defined as expertise to ongoing drug usage in order to make sure appropriate drug therapy is followed. The prescribing pattern differs from individual physician to individual patient. Prescribing is a useful tool for interaction between the physician and the patient, as well as offering the patient a written format of medication schedules.4 Hence this research is focused to assess the pattern of teneligliptin and other OADs prescribed in a clinical setting.
MATERIALS AND METHODS
Design of Study
The research is a prospective observational study carried out among patients with T2DM in a diabetic centre in Erode, India. The study was conducted with prior permission from the Institutional Human Ethics Committee (Approval ID DCC/ IEC/026/2021). The duration of the study was six months from April 2021 to September 2021. The data of patients under DPP-4i prescription were collected. All newly detected and elderly diabetic patients with gliptin and other anti-diabetic drugs between age group 18-90 years, both male and female and history of T2DM were included in the study. T1DM patients and pediatric patients and pregnant women with gestational diabetes were excluded.
Study Procedure
The study sample involved 302 patients, whose prescriptions were scrutinized and detailed information such as demography, age, sex, presenting complaints, family history, past medical history, and duration of diabetes was listed in their patient profile. Informed consent was obtained prior to the study from the patients who fulfilled the study criteria. The selected patients were then grouped based on the duration of diabetes such as (a) Newly diagnosed diabetes; (b) Duration of diabetes 1-10 yrs; (c) Duration of diabetes 11-20 yrs; (d) Duration of diabetes 21-30 yrs. The treatment regimen was also divided into four groups (i) Monotherapy; (ii) Two-drug regimen; (iii) Three-drug regimen; (iv) Four-drug regimen including insulin with other OADs. The data were collected using the case record form (CRF). The data from the CRF were transcribed onto an Excel database and analysed using SPSS statistical software. All the variables were tested for their distribution and those with normal distribution were summarized using mean and standard deviation.
RESULTS
The assessment of the prescribing pattern of the gliptin drugs for T2DM patients was performed using the data collected from 302 patients in the diabetic centre located in Erode, India. Among the 302 cases, 169 were male and 133 were female. The age group of the 302 patients of the study were in the range between 20-90 yrs, the majority of the age category in between 51-60 yrs (31.5%) and the least were in the range 80 yrs and above (1%). Approximately 269 (89.1%) patients had no physical activity and 33 (10.9%) patients were doing regular exercise. Type 2 diabetes is caused by genetic factors. Out of 302 patients, 217 (71.85%) T2DM patients have a family history of the disease and 152 (50.33%) have no family history. The study population (302) was observed with many co-morbidities. Hypertension was observed in 52 (17.2%) patients, dyslipidemia in 61 (20.2%) patients, coronary artery disease among 16 (5.3%), ischemic heart disease in 4 (1.4%) patients, anaemia with 3 (0.99%) patients, asthma and hyperthyroidism in 2 (0.66%) patients each, and COPD and Stable Angina with 1 (0.33%) patient each. Body Mass Index (BMI) values of the patients in the study were observed and found that 128 (42.38%) patients were under normal weight, 102 (33.77%) patients were overweight, 53 (17.55%) patients were obese, 14 (4.64%) patients were underweight. Among 302 patients, 76 (25.17%) were employed, 104 (34.44%) patients were self-employed, 122 (40.40%) patients were unemployed. Among the 302 patients in the study, 26 (8.6%) were prescribed monotherapy therapy, 46 (15.3%) were prescribed with the two-drug regimen, 151 (50%) patients were prescribed with the three-drug regimen and 79 (26.6%) patients were prescribed with four-drug regimen (Table 1).
| Demographic Details | Number of Patients (%) |
|---|---|
| Gender | |
| Male | 169 (55.90) |
| Female | 133 (44.10) |
| Age Group | |
| Below 30 yrs | 06 (2.00) |
| 31 to 40 yrs | 31 (10.00) |
| 41 to 50 yrs | 93 (30.80) |
| 51 to 60 yrs | 95 (31.50) |
| 61 to 70 yrs | 56 (18.50) |
| 71 to 80 yrs | 18 (60.00) |
| 81 yrs & above | 03 (10.00) |
| Below 30 yrs | 06 (2.00) |
| Physical Activity | |
| Yes | 269 (89.10%) |
| No | 33 (10.90%) |
| Family History | |
| Yes | 200 (66.20%) |
| No | 102 (33.80%) |
| Comorbid Condition | |
| Hypertension | 52 (17.20) |
| Dyslipidemia | 61 (20.20) |
| CAD | 16 (5.30) |
| COPD | 01 (0.33) |
| IHD | 04 (1.40) |
| Asthma | 02 (0.66) |
| Anaemia | 03 (0.99) |
| Hypothyroidism | 02 (0.66) |
| Stable Angina | 01 (0.33) |
| BMI | |
| Normal weight | 128 (42.38) |
| Under weight | 14 (4.64) |
| Over weight | 107 (35.43) |
| Obese | 53 (17.55) |
| Occupation | |
| Employed | 76 (25.17) |
| Self employed | 104 (34.44) |
| Unemployed | 122 (40.40) |
| Treatment Regimen | |
| Monotherapy | 26 (8.60) |
| Two drug regimen | 46 (15.23) |
| Three drug regimen | 151 (50.00) |
Among 302 patients involved in the study, the following pattern in the prescription was observed for the T2DM patients (Table 2). Teneligliptin + Metformin + Glibenclamide was prescribed for 132 (43.7%) patients. Teneligliptin + Metformin + Glibenclamide + Insulin were prescribed for 49 (16.2%) patients. Teneligliptin was prescribed as monotherapy for 26 (8.6%) patients. Teneligliptin + Metformin was prescribed for 34 (11.3%) as two-drug regimen. Teneligliptin + Glibenclamide was prescribed for 12 (04%) patients. Teneligliptin + Glibenclamide + Voglibose was prescribed for 19 (6.3%) patients. Teneligliptin + Metformin + Glibenclamide + Pioglitazone were prescribed for 30 (9.9%) patients.
| Drug prescribed | Number of patients (%) | ||||||
|---|---|---|---|---|---|---|---|
| Treatment regimen | Male | Female | Total | Statistical Inference | |||
| N | % | N | % | N | % | ||
| Teneligliptin | 15 | 8.9% | 11 | 8.3% | 26 | 8.6% | x2=18.642 Df=6 0.013* |
| Teneligliptin + Metformin | 21 | 12.4% | 13 | 9.8% | 34 | 11.3% | |
| Teneligliptin + Glibenclamide | 4 | 2.4% | 8 | 6.0% | 12 | 4.0% | |
| Teneligliptin + Metformin + Glibenclamide | 73 | 43.2% | 59 | 44.4% | 132 | 43.7% | |
| Teneligliptin + Glibenclamide + Voglibose | 9 | 5.3% | 10 | 7.5% | 19 | 6.3% | |
| Teneligliptin + Metformin + Glibenclamide + Pioglitazone | 18 | 10.7% | 12 | 9.0% | 30 | 9.9% | |
| Teneligliptin + Metformin + Glibenclamide + Insulin | 29 | 17.2% | 20 | 15.0% | 49 | 16.2% | |
| Total | 169 | 100.0% | 133 | 100.0% | 302 | 100.0% | |
Diabetic duration was statistically significant with the treatment regimens (p<0.05), indicating that the diabetes duration increased due to uncontrolled conditions leading to three/four drug regimen prescription. The current study was found to include a maximum three drug regimen (Table 3).
| Diabetic History | N | Mean | S.D. | SS | Df | MS | Statistical Inference |
|---|---|---|---|---|---|---|---|
| Between Groups | 682.660 | 6 | 113.777 | F= 3.424 0.003* | |||
| Teneligliptin | 26 | 4.69 | 4.897 | ||||
| Teneligliptin + Metformin | 34 | 6.03 | 5.480 | ||||
| Teneligliptin + Glibenclamide | 12 | 4.17 | 3.129 | ||||
| Teneligliptin + Metformin + Glibenclamide | 132 | 6.98 | 5.638 | ||||
| Teneligliptin + Glibenclamide + Voglibose | 19 | 9.26 | 7.709 | ||||
| Teneligliptin + Metformin + Glibenclamide + Pioglitazone | 30 | 9.63 | 6.111 | ||||
| Teneligliptin + Metformin + Glibenclamide + Insulin | 49 | 8.61 | 6.103 | ||||
| Teneligliptin | 302 | 7.24 | 5.902 | ||||
| Within Groups | 9802.662 | 295 | 33.229 |
DISCUSSION
This study analysed the prescribing pattern of Teneligliptin in T2DM patients in a diabetic centre located. It was observed in the study that most of the population were males compared to females. This study shows that there is a statistically significant difference between the treatment regimen and the male-female ratio (p<0.05). Social habits and lifestyle changes may be the cause for a male being more affected than the female.10
In the study, one-third of the population was in the age group of 51-60 years, and do indeed have a high prevalence of diabetes. T2DM prevalence increases with age. Similar results were observed in the study by Mohammad A et al., suggesting majority of the diabetic patients were in the age groups of 41-60 years.11 The reason is that ageing causes interference in glucose metabolism leading to a decline in insulin production with respect to glucose concentration, and also there is insulin resistance in endothelial cells. Insulin level declines with age and obesity.12
Diabetes Mellitus is exacerbated by combination of genetic and environmental factors. In the present study, Most of the patients have a family history of T2DM. Jonathan Q. Purnell et al., concluded that the patients having a family history of Type 2 diabetes had increased central weight gain and hyperlipidemia, as measured by greater levels of triglyceride and higher levels of cholesterol in intermediate-density lipoproteins and VLDLs, than patients without a family history. In T1DM and T2DM, antibodies acting against GAD65 and insulinoma-associated protein 2 (IA-2) are useful disease markers.13 Among the study population, a higher number of patients had dyslipidemia followed by hypertension. The predominance of dyslipidemia and hypertension is higher in diabetic patients. This may be due to the metabolic action of insulin, which secondarily influences the metabolism of the body. Hurst C et al., also showed that the majority of patients had hypertension as the main comorbidity.14
Body Mass Index (BMI) values of the patients in the current research revealed that 107 patients were overweight and 53 patients were obese. Obesity is the most common complication in T2DM patients and promotes insulin resistance. Exercise and diet on a regular basis for losing weight may assist to enhance tissue sensitivity to insulin. DPP4i was prescribed for most of overweight and obese patients since they have a weight-neutral effect.15, 16
In the current study, most of the patients belong to low-income and middle-income category. Teneligliptin has low cost than the other DPP-4i and is affordable by all the category patients. Tandon T et al. stated in their study that the combination therapy of metformin and glimepride for T2DM patients is significant and much cost-effective than metformin and teneligliptin in terms of lowering HbA1c and FPG.17 Contradictorily, the current study reveals teneligliptin to be cost-effective as monotherapy.
Most of the patients in the study were prescribed with three drug regimens, since there was prevalence of high blood glucose level due to highly rich carbohydrate food, lifestyle changes and lack of physical activities. Misbahuddin MR et al. stated that the percentage of patients on triple combination therapy was low.18 The present study concludes that the current lifestyle modifications with single-drug therapy alone cannot achieve good glycaemic control in uncontrolled T2DM.
Among 302 patients in the study, most of the patients were prescribed Teneligliptin + Metformin + Glibenclamide and few were prescribed with Teneligliptin + Glibenclamide + Voglibose.
In the present study, the guidelines by Indian Council for Medical Research (ICMR) were implemented for the judicious use of medication as the prescribing pattern was followed. Metformin has been the most preferred antidiabetic medicine in all diabetes categories. As a second-line medication after metformin, DPP-4i seems to rapidly catch up with sulfonylurea. Most patients demand insulin therapy for their glycemic control which in turn increases the duration of diabetes. Glimepiride with metformin was a widely used combination of medication.19, 20
In the study, there is association between the types of drugs prescribed and duration of diabetes. Diabetes duration plays an important role in management of hyperglycaemia. Diabetes with a period of fewer than 5 years has typically been controlled with single-drug therapy, and an increasing number of drugs are required in cases of extended duration of diabetes with uncontrolled diabetic conditions. The development from normal glucose tolerance to diabetes is characterized by a decline in beta-cell mass, which gives rise to impaired ß-cell activity, and eventually results in glucotoxicity, which may be a known cause of apoptotic cell death, likely to result throughout ß-cell proliferation deficiencies. As a result, having diabetes for a longer period of time, especially with poor glycemic control, is likely to impair the function of ß-cell and also increases the chances of insulin therapy.21 Type 2 diabetes with a longer duration of disorder needed complex diabetes drug regimens.
CONCLUSION
The current study concludes that the current lifestyle modifications with single-drug therapy alone cannot achieve good glycaemic control in uncontrolled T2DM. So, a two-drug regimen is selected among the sulfonylureas, thiazolidinediones and DPP-4i. To avoid therapeutic inertia, newer drugs including Teneligliptin along with other DPP-4i as combination therapy are prescribed more commonly to sustain glycemic control. Another important criterion is the duration of diabetes which states that increased diabetes duration altered the treatment regimen.
References
- Rajendra P, Viswanathan M. Epidemiology of type 2 diabetes in India. Indian J Ophthalmol. 2021;69(11):2932-2938. [CrossRef] | [Google Scholar]
- Kyrou I, Tsigos C, Mavrogianni C. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC EndocrDisord. 2020;20(1):134 [CrossRef] | [Google Scholar]
- [CrossRef] | [Google Scholar]
- [CrossRef] | [Google Scholar]
- Karimi A, Haerizadeh M, Soleymani F, Haerizadeh M, Taheri F. Evaluation of medicine prescription pattern using World Health Organization prescribing indicators in Iran: A cross-sectional study. J Res Pharm Pract. 2014;3(2):39-45. [CrossRef] | [Google Scholar]
- Elnaem M, Shamsuri MHH, Mohamad Aziz NA, Alias NI, Hafizi RF, Latif NF, et al. prescribing pattern of dipeptidyl peptidase 4 inhibitors and level of HBA1c target achievements among outpatients with type 2 diabetes mellitus in a Malaysian university teaching hospital. Romanian J Diabetes Nutr Metab Dis. 2020;27(4):396-302. [CrossRef] | [Google Scholar]
- Hemant T, Jothydev K, Shahu I, Ruchi S, Rishi J. Comparison of efficacy and safety of teneligliptin and glimepride as add-on to metformin in ameliorating glycemic variability based on professional continuous glucose monitoring data in patients with type 2 diabetes mellitus. Int J Curr Res. 2019;11(7):279-84. [CrossRef] | [Google Scholar]
- Cignarella A, Bolego C. Mechanisms of estrogen protection in diabetes and metabolic disease. Horm Mol Biol Clin Investig. 2010;4(2):575-80. [PubMed] | [CrossRef] | [Google Scholar]
- Karimi A, Haerizadeh M, Soleymani F, Haerizadeh M, Taheri F. Evaluation of medicine prescription pattern using World Health Organization prescribing indicators in Iran: A cross-sectional study. J Res Pharm Pract. 2014;3(2):39-45. [CrossRef] | [Google Scholar]
- Mushtaq S, Mayee KR, Amreen S, Satyanarayana V, Yerramilli A, Ramakrishnan S, et al. A study on the current prescribing patterns of Dipeptidyl peptidase 4 inhibitors in a multi–Speciality Hospital Outpatient Setting. Asian J Pharm Clin Res. 2014;7(7):134-6. [CrossRef] | [Google Scholar]
- Mohammad A, Imran A K, Vinay V S, Najnin K, ZahiruddinQuazi Syed E. Evaluation of the diabetic foot according to Wagner’s classification in a rural teaching hospital. Br J Diabetes Vasc Dis.. 2011;11:74-79. [CrossRef] | [Google Scholar]
- Chee W, Josephine M, Luigi F.. Age-related Changes in Glucose Metabolism, Hyperglycemia, and Cardiovascular Risk. Circ Res.. 2018;123(7):886-904. [CrossRef] | [Google Scholar]
- Purnell JQ, Dev RK, Steffes MW, Cleary PA, Palmer JP, Hirsch IB, et al. Relationship of family history of type 2 diabetes, hypoglycemia, and autoantibodies to weight gain and lipids with intensive and conventional therapy in the Diabetes Control and Complications Trial. Diabetes. 2003;52(10):2623-9. [CrossRef] | [Google Scholar]
- Hurst C, Thinkhamrop B, Tran HT. [2015 Oct 22];The Association between Hypertension Comorbidity and Microvascular Complications in Type 2 Diabetes Patients: A Nationwide Cross-Sectional Study in Thailand. Diabetes Metab J. 2015;39(5):395-404. [CrossRef] | [Google Scholar]
- Sesti G, Avogaro A, Belcastro S, Bonora BM, Croci M, Daniele G, et al. Ten years of experience with DPP-4 inhibitors for the treatment of type 2 diabetes mellitus. Acta Diabetol. 2019;56(6):605-17. [CrossRef] | [Google Scholar]
- Makrilakis K. The Role of DPP-4 Inhibitors in the Treatment Algorithm of Type 2 Diabetes Mellitus: When to Select, What to Expect. Int J Environ Res Public Health. 2019;16(15):2720 [CrossRef] | [Google Scholar]
- Tandon T, Dubey AK, Srivastava S, Manocha S, Arora E, Hasan N, et al. A pharmacoeconomic analysis to compare cost-effectiveness of metformin plus teneligliptin with metformin plus glimepiride in patients of type-2 diabetes mellitus. J Family Med Prim Care. 2019;8(3):955-9. [CrossRef] | [Google Scholar]
- Misbahuddin MR, Hussam AM, Zohair JG, Ziaullah MS. Anti-diabetic drug utilization patterns in a government hospital in Saudi Arabia. Trop J Pharm Res. 2018;7(6):1193-200. [CrossRef] | [Google Scholar]
- Himani G, Seema G, Vivek M, Nusrat Kareem, Suman Kumar K. Prescribing Pattern of Drugs in Outdoor Patients with Type 2 Diabetes Mellitus in Relation to the Duration of Diabetes in a Tertiary Care Teaching Hospital – A Prospective Observational Study. J Evid Based Med Healthcare. 2021;8(5):256-60. [CrossRef] | [Google Scholar]
- Akmal Alibaig M, GirendraKumar G. Assessment of current prescribing pattern and cost analysis of oral antidiabetic drugs in elderly population from Punganur region of Andhra Pradesh. Int J Pharm Pharm Sci. 2021;13(7):32-9. [CrossRef] | [Google Scholar]
- . Duration of diabetes and types of diabetes therapy in Japanese patients with type 2 diabetes: The Japan Diabetes Complication and its Prevention prospective study 3 (JDCP study 3). J Diabetes Investig. 2017;8(2):243-9. [CrossRef] | [Google Scholar]
