ABSTRACT
Background
The most prevalent fungus infections that adversely affect people of all ages are called dermatophytoses. It is brought on by a particular class of fungus called ringworms, sometimes known as tineas, which includes the species Microsporum, Trichophyton, and Epidermophyton. About 20–25% of people worldwide have dermatophytosis. Direct contact with sick people can spread the disease, as can indirect contact with contaminated fomites. To determine the epidemiology, risk factors, clinical trends, and treatment profile of Superficial Fungal Infections, the current investigation was conducted (SFIs).
Materials and Methods
A hospital-based prospective observational cross-sectional study was carried out at RIMS, Kadapa for six months, from November 2021 to April 2022. Based on the inclusion criteria, 120 patients were chosen. Data was gathered, examined, and summarized as averages. Microsoft Excel was used to represent the data using the graph pad prism programme.
Results
In a total of 120 patients with tinea infections, we discovered that 45 were men and 75 were women; 64 patients are in the middle age group; 51 had BMI values below 18.5; 73 are illiterate; 15 have social habits; 60 are housewives; and 93 got Tinea as a result of towel sharing. In 87 patients with Tinea corporis, the upper and lower limbs were frequently afflicted; Trichophyton rubrum was isolated in 97 cases. There were 527 prescriptions total, of which 315 were for oral treatments and 212 were for topical treatments.
Conclusion
Tinea corporis was the most common superficial fungal infection found in the GGH-RIMS. The most frequent species of Trichophyton isolated from patients with tinea was Trichophyton rubrum. Both the antifungal drug miconazole and the antihistamine drug CPM were widely prescribed.
INTRODUCTION
The most prevalent fungi that have a negative impact on people of all ages and their quality of life are cutaneous mycoses. An estimated 20–25% of people worldwide are thought to be affected by superficial fungal infections.1 The fungus known as dermatophytes, which need keratin to develop, infect the epidermis and keratin-rich tissues like the hair and nails, resulting in tinea. Dermatophytoses, often known as ringworms or tineas, are dermatomycoses that are brought on by a particular class of fungi that includes the species Microsporum, Trichophyton, and Epidermophyton.2 A species is said to as geophilic, zoophilic, or anthropophilic depending on whether it lives in dirt, animals, or people. Direct contact with sick people can spread the disease, as can indirect contact with contaminated fomites.3
Incubation lasts one to two weeks in humans. Infection with dermatophytes is quite frequent everywhere. Due to the risk factors of overcrowding, low socioeconomic level, and poor personal cleanliness, it occurs more frequently in poorer nations. Tinea pedis, Tinea cruris, and onychomycosis are more prevalent in adolescents than tinea capitis, tinea corporis, and tinea pedis are in prepubescent children. Only two geophilic dermatophytes—Microsporum gypseum and Microsporum mannum—are significant animal pathogens. The most common dermatophytes involved in human cases vary according to the climate, geographic region, and additional elements like exposure to domestic or exotic animals.4
Sharing footwear, clothing, and towels frequently helps spread infections among family members. These items, together with clothing, bedsheets, and towels, harbour fungus germs that can cause disease. Wearing restrictive clothing, such as jeans and underwear, throughout the winter months that were sometimes left unwashed for weeks, creating a moist environment that was conducive to the growth of dermatophytes.5 Infections are mostly disseminated through anthropophilic, geophilic, and zoophilic factors. The ring-shaped dermatophytosis lesion, also known as a ring worm lesion, typically has inflammatory edges and a clear, normal-looking centre. Due to high temperatures and humidity, dermatophytes are the most frequent agents that result in superficial fungal infections around the world, particularly in tropical and subtropical nations like India. Studies on the epidemiology of dermatophyte infections from various regions of India over the past several years have revealed an increase in the prevalence of cutaneous dermatophytosis along with changes in the spectrum of infection and the isolation of rare species.6
The World Health Organization (WHO) reports that 30% to 70% of persons in the world are asymptomatic carriers of dermatophytoses, which impact roughly 25% of the global population. Numerous variables, including the tropical environment, overcrowding, urbanization, shared housing, such as hostels, the use of occlusive footwear, tight-fitting clothing, public baths, and sports activity, have been linked to the increased prevalence of dermatophytosis.7 Physical examination and laboratory testing can be used to diagnose these superficial dermatophyte infections. KOH 10- 20% treatment of skin samples is a quick and affordable bedside method to provide evidence of dermatophyte infections. The most used isolation medium for dermatophytosis is Sabourauds Dextrose Agar (SDA), which contains 4% peptone, 1% glucose, agar, and water. This medium provides the foundation for most morphologic studies. Colony development takes 7–14 days.8
There are numerous therapeutic approaches that can be employed as sequential therapy, combination therapy, or monotherapy. Due to their heightened susceptibility to undesirable adverse effects, specific patient populations, such as pregnant women, children, and the elderly, frequently require customized treatment algorithms. The type of infection and the symptom are the key determinants of therapy length. Typically, skin lesions require treatment for three weeks, while foot irritation requires treatment for six weeks. Dermatophytosis treatment is normally a time-consuming and difficult process that typically involves the use of azoles and anti-fungal medications of the allyl amine class (such as Terbinafine) (Ketoconazole, Miconazole, Oxiconazole). In comparison to therapy with the fungi-static azoles, topical therapy with fungicidal allyl amine anti-fungal is associated with somewhat higher cure rates and shorter treatment courses. Topical treatment typically works for dermatophyte infections. Applying lotions or sprays rather than creams to large or hairy regions is simpler.9 Among the topical antifungals are: Clotrimazole – cream 1%, Miconazole – cream 2%, Econazole – cream 1%, Ketoconazole – cream 2%, Oxiconazole – cream 1%, Terbinafine – cream 1%, Butenafine – cream 1%. Majocchi granuloma is an uncommon consequence in which the dermatophyte penetrates further into the dermis or subcutaneous tissue through a follicle. When treating Majocchi granuloma, oral antifungals like terbinafine 250 mg once daily for 2 to 4 weeks are advised. The erythematous nodules or papules that represent lesions are those that affect the hair follicles. These could potentially develop into abscesses. When treating Majocchi granuloma, oral antifungals like terbinafine 250 mg once daily for 2 to 4 weeks are advised.10 The major aim of our study is to find out epidemiology, risk factors, clinical patterns and therapeutic profile of dermatophytosis among adults consulting dermatology OPD in a tertiary care teaching hospital.
MATERIALS AND METHODS
A prospective observational study was carried out by collecting the data in designed form, from OPD dermatology, at GGH-RIMS, Kadapa, Andhra Pradesh. During the 6 months’ study period, a total of 120 patients were recruited. Patients who agreed to participate in study by signing informed consent form were enrolled. Skin samples, hair samples and nail samples from clinically diagnosed dermatophytosis cases for KOH mount and fungus culture was done. In addition, detailed history also taken focusing on possible risk factors (contact with pet animals, family history) that increase in the occurrence of dermatophytosis. Permission for collecting patient’s data was approved by Institutional Ethical Committee of RIMS hospital (PRRMCP/IEC/2021/11/03; Dated: 10.02.2022). Both male and female patients of age groups of 10 to 70 years and patients with a confirmatory diagnosis of dermatophyte infections, those suffering from contagious dermatophytosis were included in this study. Patients who were not willing to participate, pregnant and breast feeding women, neonates, children, geriatrics (> 70 years) and patients with incomplete data and inconsistent diagnosis of dermatophytosis, those who were prescribed antibiotics along with antifungals for prophylaxis, and taking alternative systems of medications (except Allopathy) were excluded from this study.
All the prescriptions containing anti-fungal drug regimens were monitored closely to know the frequency and the extent to which antifungals were indicated to treat dermatophyte infections. Statistical averages were considered for the evaluation of patients’ data. Results were represented as frequencies, and percentages. Graphpad Prism software was applied to analyze the data. Bar graphs and pie charts were framed by using Microsoft Excel. The detailed workflow of the study has been depicted in the Figure 1.
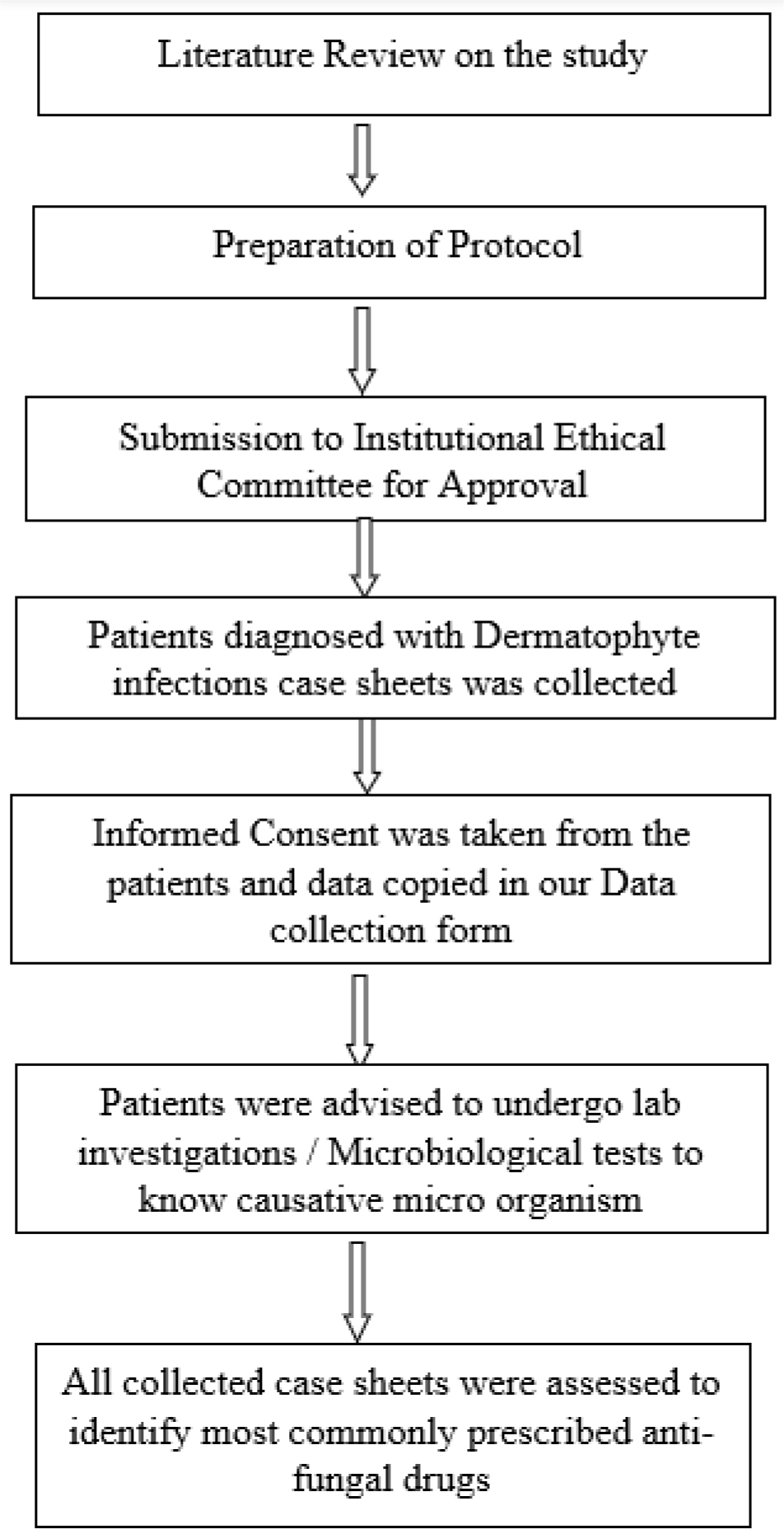
Figure 1:
Flow chart of the study.
RESULTS
Socio-demographic characteristics
Data from 120 patients who had Dermatophytosis are recruited for this study. Of these, 45 (37.5%) were males and 75 (62.5%) patients were females with a sex ratio of 3:5 (M: F). The majority of patients 36 (30%) belonged to the age group of 31 to 40 years. On the basis of education, most of the patients (73, 61%) were illiterates. Taking occupation into consideration, we found that 60 patients i.e., 50% were stay-at-home mothers are summarized in below Table 1.
| Patient demographic details | Frequency | Percentage (%) |
|---|---|---|
| Gender Males Females Mean ± SD | 45 75 60 ± 21.2132 | 37.5 62.5 |
| Age groups 11-20 21-30 31-40 41-50 51-60 61-70 Mean ± SD | 24 23 36 28 8 1 20 ±13.0384 | 20 19.93 30 23.33 6.66 0.08 |
| Education Below SSC SSC HSC Graduate Post graduate Mean ± SD | 73 9 5 32 1 24±29.91655 | 60.83 7.5 4.93 26.66 0.08 |
| Occupation Home-makers Students Daily wage workers Farmers Monthly employers Mean ± SD | 60 31 18 4 7 24±22.74863 | 50 25.83 15 3.33 5.84 |
Type of Dermatophyte diagnosis
According to the results of the current research, out of 120 patients, 87 (72.5%) had Tinea corporis, followed by 11 (9.1%) with tinea corporis and cruris, 10 (8.4%) with Tinea incognito, 7 (5.8%) with Tinea cruris, 2 (1.7%) with Tinea faciei, and 1 (0.8%) with Tinea corporis was the diagnosis with the highest prevalence of superficial fungal infections, as depicted in Table 2.
| Type of dermatophytosis | Frequency | Percentage (%) |
|---|---|---|
| Tinea corporis Tinea corporis and cruris Tinea incognito Tinea cruris Tinea faciei Tinea barbae Tinea pedis Mean ± SD | 87 11 10 7 2 2 1 17.14286±31.06675 | 72.5 9.1 8.4 5.8 1.7 1.7 0.8 |
Isolation of micro-organisms
Utilizing cultural and morphological traits such colony development pattern, conidial morphology, and pigmentation, the fungal isolates were identified. Regularly, cultures are kept at 25° to 30° C for up to 4 weeks. Sabouraud’s Dextrose Agar (SDA), which has an acidic pH, is a typical media for fungus cultivation (of 5.6). In our investigation, Trichophyton rubrum, which makes up 97 (81%), Trichophyton mentagrophytes, which makes up 15%, Microsporum audouinii, which makes up 6%, and Microsporum gypseum, which makes up 2%, were all detected. Trichophyton rubrum was the most often isolated species, details are clearly shown in Table 3.
| Name of isolated micro-organisms | Frequency | Percentages (%) |
|---|---|---|
| T. rubrum T. mentagrophytes M. audouinii M. gypseum Mean ± SD | 97 15 5 2 29.75 ± 45.17651 | 81% 12% 4% 2% |
Management of Dermatophyte infections
The total number of medications prescribed-527-in the 120 prescriptions included the following dosage types. 209 cures (39.66%) were 4 (5.1) creams, 315 (59.77%) were pills, and 1 (0.19%) used lotion, soap, and shampoo. The most frequently prescribed dose form was the pill. Oral antifungals and antihistamines are both available as tablets. A total of 527 prescriptions were prescribed, of which 203 (38.50%) were antihistamines, 112 (21.30%) were oral antifungals, 209 (39.65%) were topical antifungals, 2 (0.37%) were topical steroids, and 1 (0.18%) was an emollient. Topical antifungals made up the majority of the medications a dermatologist prescribed in our study, and the tinea patients who underwent treatment did not receive any of the vitamin supplements. Azole medications (321 in total), such as miconazole (111), clotrimazole (95), fluconazole (73), itraconazole (39), ketoconazole (2), and luliconazole (1), were more frequently prescribed than antihistamines (203 in total), such as cetirizine (88) and CPM (115). All these particulars are represented in Table 4.
| Drug category | Frequency | Percentage (%) |
|---|---|---|
| Oral antihistamines Oral antifungals Topical antifungals Topical steroids Emollients Vitamin supplements Mean ± SD | 203 112 209 2 1 0 105.4±102.3391 | 38.50 21.30 39.65 0.37 0.18 0 |
DISCUSSION
The majority of superficial fungal infections are caused by dermatophytes. Their special capacity to break down keratin sets them apart from other pathogenic filamentous fungi in terms of pathological activity. Dermatophytes are pathogenic fungi that have a strong preference for the keratinized tissues found in skin, hair, and nails. They are responsible for the surface infections known as Dermatophytoses. This group of mushrooms has an exceptional capacity for adaptability to changing environmental conditions, which is shown in the diversity of their morphology and ecology. The frequency of dermatophyte infections is more common in girls than in men, with a female-to-male ratio of 5:3, according to extensive research conducted at the study location. The ratio of female to male patients at the skin OPD at Indira Gandhi Medical College and Employees State Insurance Hospital in the state of Himachal Pradesh was 5:3, indicating a rising frequency of tinea infections in women, according to a study by Prakash Chand Sharma and colleagues.5
37% of the participants in the current study were men and 63% were women, showing a gender imbalance. According to a 2012 study by Costa Orlandi et al., female patients were more likely than male patients to reach the same findings (146, or 77.2% versus 43, or 22.8%).11 Homemakers (50%) and students (24.05%) were the most often impacted groups, followed by daily wage workers (15%). In a tertiary care hospital, Vegada et al., conducted a study that had uniform results and primarily affected homemakers.12
We found that frequent towel sharing contributed to the transmission of infection in 93 patients, followed by clothing sharing in 38 patients, in a total of 120 cases. Clothes, bedsheets, and towels are examples of items that carry the fungus infections and can spread the illness to family members. Out of 187 subjects, 97 patients exchanged towels, which has been implicated in the transmission of dermatophyte infection from person to person. This finding could be a sign that enhanced human-to-human transmission could improve the aggressiveness of diseases, according to a 2009 study by Das et al.13 Tinea corporis (72.5%) was the most prevalent clinical form, followed by a mix of tinea corporis and cruris (9.1%). Similar findings, i.e., a diagnosis percentage of (29.1%) for Tinea Corporis, were found in research conducted by Paudel et al.14
Trichophyton rubrum, which accounted for 81% of the isolated causal agents in the current investigation that caused dermatophytosis, was followed by Trichophyton mentagrophytes. Seebacher et al. 2008’s review study included the same information, which is 80–90% of the commonly isolated T. rubrum species, followed by T. mentagrophytes. The most prevalent species, according to a 1999 study by Nita Patwardhan et al., was T. rubrum (28.12%). During the course of our inquiry, it became clear that dermatologists were restricted to hospital formularies. Pharmaceuticals were prescribed 99.62% by generic name and 0.38 % by brand name. According to Preety Bansal’s review research, generic drug prescriptions predominate (50.33%), while pharmaceuticals from the NLEM (National List of Essential Medicine) account for 20.93% of all prescriptions. The WHO estimates that 100% of medications are prescribed under their generic names. As a result, our research proposal complies with the WHO benchmark value for generic medicine utilization. Prescriptions for topical dose forms (40%) are almost identical to those for oral dosage forms (tablets) (60%), according to our research proposal. Azole medications (321 in total), such as miconazole (111), clotrimazole (95), fluconazole (73), itraconazole (39), ketoconazole (2), and luliconazole (1), were more frequently prescribed than antihistamines (203 in total), such as cetrizine (88) and CPM (115). Acsah George et al. in 2018 provided evidence to support this claim that azoles were the most often utilised topical antifungals. In a separate study published in 2018 by Muralidhar Rajagopalan et al, researchers found that specialists generally concurred that topical azoles should be used as an initial course of treatment for tinea infections.
3.3 medications were often prescribed for each prescription, regardless of the dosage form. It was related to a 2015 study by Anuj Kumar Pathak et al. in which they found that the typical number of medications prescribed was 5.13. The sum did not match, which can be because different doctors have different prescribing habits.15
It is clear from the foregoing that tinea infections are frequent dermatological conditions at GGH-RIMS, Kadapa. Our results might point to an epidemiological shift that necessitates more investigation. Preventable actions, such as screening by a health team and the use of educational programs to increase health literacy among society’s members, could aid in reducing risk factors for fungal infections in the future, such as poor personal cleanliness, contact with pets, and crowding.
CONCLUSION
In India, dermatophytosis is fairly typical. The combination of a hot, humid climate and bad hygiene is very conducive to the growth of fungi. The frequency of dermatophyte infections is more common in girls than in men, with a female-to-male ratio of 5:3, according to extensive research at our study location. When compared to underdeveloped countries, its prevalence has considerably decreased in many industrialized countries because of better social, economic, health care, and cleanliness practices. The characteristics of the infecting organisms and the accessibility of control methods are the main causes of these variations in the prevalence of infection in various locations. Our study also highlighted the need for patient counselling by raising awareness of the condition, its causes, and the risk factors that may lead to its occurrence. Sharing infected personal items and close contact should be avoided to stop the spread of an infection. To understand the severity of the infection and its progression, knowledge of the common fungi in the area is crucial.
Recommendation
Recommended first-line topical therapy is Terbinafine 1% cream once or twice daily for one to two weeks. The cure rates for laser therapy in onychomycosis are significantly lower than topical and oral therapies. Given its limited efficacy and high cost, laser therapy cannot be recommended as a first-line treatment for onychomycosis.
Limitation
The microbiology department should be strengthened in such a way that patients collect their culture reports within the timeline that helps the dermatologists to prescribe antifungals rationally. The present study was conducted for a short period of time with limited sample size and there is no follow up of the patients to correlate the results of the anti-fungal susceptibility and clinical outcomes.
References
- Peres NT, Maranhão FC, Rossi A, Martinez-Rossi NM. Dermatophytes: host-pathogen interaction and antifungal resistance. An Bras Dermatol.. 2010;85(5):657-67. [PubMed] | [CrossRef] | [Google Scholar]
- [PubMed] | [CrossRef] | [Google Scholar]
- Degreef H. Clinical forms of dermatophytosis (ringworm infection). Mycopathologia. 2008;166(5-6):257-65. [PubMed] | [CrossRef] | [Google Scholar]
- Oros J, Calabuig P, Arencibia A, Camacho M, Jensen H. Systemic mycosis caused by Trichophyton spp. in an olive Ridley sea turtle (): an immunohistochemical study. N Z Vet J. 2011;59(2):92-5. [PubMed] | [CrossRef] | [Google Scholar]
- Bhatia VK, Sharma PC. Epidemiological studies on Dermatophytosis in human patients in Himachal Pradesh, India. Springerplus. 2014;3:134 [PubMed] | [CrossRef] | [Google Scholar]
- Lakshmanan A, Ganeshkumar P, Mohan SR, Hemamalini M, Madhavan R. Epidemiological and clinical pattern of dermatomycoses in rural India. Indian J Med Microbiol.. 2015;33:S134-6. [PubMed] | [CrossRef] | [Google Scholar]
- Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995;8(2):240-59. [PubMed] | [CrossRef] | [Google Scholar]
- Singh J, Zaman M, Gupta AK. Evaluation of microdilution and disk diffusion methods for antifungal susceptibility testing of dermatophytes. Med Mycol. 2007;45(7):595-602. [PubMed] | [CrossRef] | [Google Scholar]
- Sahoo AK, Mahajan R. Management of Tinea corporis, Tinea cruris, and Tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86. [PubMed] | [CrossRef] | [Google Scholar]
- Elgart ML. Tinea incognito: an update on Majocchi granuloma. Dermatol Clin. 1996;14(1):51-5. [PubMed] | [CrossRef] | [Google Scholar]
- Costa-Orlandi CB, Magalhães GM, Oliveira MB, Taylor EL, Marques CR, de Resende-Stoianoff MA, et al. Prevalence of dermatomycosis in a Brazilian tertiary care hospital. Mycopathologia. 2012;174(5-6):489-97. [PubMed] | [CrossRef] | [Google Scholar]
- Vegada BN, Karelia BN, Singh AP. Drug utilization study of antifungal agents used in department of skin and VD of a tertiary care teaching hospital. Int J Pharm Sci. 2015;34(1):118-21. [PubMed] | [CrossRef] | [Google Scholar]
- Das K, Basak S, Ray S. A study on superficial fungal infection from West Bengal: A brief report. J Life Sci. 2009;1(1):51-5. [CrossRef] | [Google Scholar]
- Paudel D, Manandhar S. Dermatophytic infections among the patients attending di skin hospital and research center at Maharajgunj Kathmandu. J Nepal Health Res Counc. 2015;13(31):226-32. [PubMed] | [Google Scholar]
- Pathak AK, Kumar S, Kumar M, Mohan L, Dikshit H. Study of drug utilization pattern for skin diseases in dermatology OPD of an Indian tertiary Care Hospital – A prescription survey. J Clin Diagn Res. 2016;10(2):FC01-5 [PubMed] | [CrossRef] | [Google Scholar]
