ABSTRACT
Background
Lumbosacral Transitional Vertebrae (LSTV) is one the common spinal anomalies encountered in patients with low backache. The aetiology of back pain is idiopathic, however low back ache causes substantial loss of productivity. LSTVs include various types such as Lumbarization, Sacralization, and the vertebrae with morphology such as complete fusion to the broadened transverse process. Low back pain associated with LSTV is due to anomalous articulation or may arise from the level above the transition, the contralateral facet when unilateral. Hence, the present study is planned to assess the prevalence of subtypes of LSTV in patients with low back aches and to determine the association of the different subtypes of LSTV with low back pain in a South Indian population.
Materials and Methods
In this study, data was collected from 1000 patients of both sex in the age group of 15 to 90 years with complaints of low back ache attending the outpatient department of Orthopaedics of Saveetha Medical College, Chennai. The patients were sent to the Department of Radiology where radiographic images of the lumbar spine, anteroposterior view, and transverse view were taken. The patients were clinically and radiologically assessed and documented.
Results
Out of the 1000 patients with complaints of low back ache, the incidence was more common in females (51.5%), than in males (48.5%). 155 patients in the study population showed imaging features of LSTV in which 24 (15.5%) showed Castellvi type I, 88 (56.7%) showed Castellvi type II, 18 (11.6%) had Castellvi type Type III and 25 (16.1%) showed Castellvi type IV. Out of these patients, type IA was observed in 13.1% and type IB in 2.5%. Maximum exhibited Castellvi type II in which type IIA was 22.2% and type IIB was 34.5%. Among Castellvi type III, 6.4% exhibited type IIIA, 5.2% type IIIB and 16.1% showed Castellvi type IV.
Conclusion
Our study shows the association of LSTV type II with low back pain with more prevalence of low back pain noted in females. Therefore, LSTV should be considered part of the differential diagnosis of back pain, especially in cases of refractory pain.
INTRODUCTION
Lumbosacral Transitional Vertebrae (LSTV) is an anomalous vertebra with intermediate morphologic characteristics between the sacral and the lumbar vertebrae1,2 its transverse processes are enlarged and can articulate with the sacrum or the ilium.3 The association between LSTV and low back ache has been disputed for a long and is generally known as Bertolotti’s syndrome.4,5 The resulting combination of attributes has a mixture of lumbar and sacral spine resulting in Lumbar sacral transitional vertebrae. Lumbarization means a caudal shift of the first sacral segment which assumes some characteristics of the lumbar vertebra.3,4 Sacralization means a cranial shift where the last lumbar vertebra assumes sacral characteristics and frequently becomes incorporated into the sacrum.6 Depending on the direction of the shift, the affected patient may have significant biomechanical and clinical implications.7 Studies have shown that there are many reasons supporting the possibility of transitional vertebra being associated with Low Back Pain (LBP). The suspected causes are spinal stenosis, disc degeneration, disc prolapse, olisthesis, muscle strain or sprain, sacroiliac joint pain, chemical irritation and nerve impingement.8,9 Due to the common presentation of low back pain and its multifactorial causes as observed in the populace, it is necessary to identify the cause for low back pain due to transverse mega-apophysis contact with the sacrum and differentiate it from back pain in patients with LSTV.10 Pain in the presence of an LSTV may also arise from disc herniation or degeneration, facet joint arthrosis, spinal canal or foraminal stenosis.8 In many patients the exact cause is unclear.11 The above-mentioned suspected causes could be due to the presence of LSTV. According to Castellvi, LSTV is divided into 4 types.12 Though the presence of an LSTV disrupts normal spine biomechanics, reduction of muscle volume and is associated with low back pain still conflicting reports exist about whether LSTV could cause low back aches or not.13,14
So, the objective of the study was to assess the prevalence of transitional vertebrae and their role in the etiopathogenesis of low back ache among the south Indian population.
MATERIALS AND METHODS
In this prospective cross-sectional study, data was collected from 1000 patients in the age group of 15 to 90 years with complaints of low back ache attending the outpatient department of Orthopaedics of Saveetha Medical College, Chennai. The patients were sent to the Department of Radiology where radiographic images of the lumbar spine, anteroposterior view, and transverse view were taken. The patients were clinically and radiologically assessed and documented.
Radiographs belonging to both sexes from the states of Tamil Nadu, Kerala, Karnataka, Andhra Pradesh, and Telangana with complaints of low back pain were included in the study. Post-traumatic patients with lumbar and sacral vertebral fractures, pregnant women, and prior history of surgery to the lower lumbar region were excluded.
Institutional ethical committee approval and written informed consent of the patient for participation in the study was obtained. All radiological images used in the study were anonymized by removing patient identifiers. The diameter of the bilateral transverse processes of the L5 lumbar vertebra, as assessed on AP lumbosacral spine X-rays, was one of the criteria used to determine the presence of LSTV. If present, the Castellvi radiographic categorization was applied to further categorize the LSTV into four kinds.12 Castellvi classification of Lumbosacral transitional vertebra is presented in Table 1.12
| Castellvi Type | Definition |
|---|---|
| LSTV type I: A-Unilateral, B-Bilateral. | The dysplastic transverse process with height > 19 mm. |
| LSTV type II: incomplete Lumbarization/sacralisation. A-Unilateral, B-Bilateral. | Enlarged transverse process with pseudoarthrosis with adjacent sacral ala. |
| LSTV type III: complete Lumbarization / sacralisation. A-Unilateral, B-Bilateral. | Enlarged transverse process which has a complete fusion with adjacent sacred ala. |
| LSTV type IV: mixed. | Type II on one side and Type III on other. |
Radiographs were obtained by digital radiography using a computed radiography system with Allengers 650 ma X-ray machine. The factors kept for image acquisition were (a) KVp- 80 mAs- 45 for AP projection and (b) KVp – 80 mAs – 140 for lateral projection. Two radiologists with a combined experience of more than ten years interpreted and classified plain radiographs using the Castellvi radiographic categorization method.
RESULTS
Among 1000 patients with complaints of low back ache, 51.5% were females, 48.5% were males and 155 (15.5%) exhibited LSTV features. Of the 155 patients, 4% were in the age group of 15 to 20yrs, 47.5% were in 21-40 years of age, 40.5% were in 41-60 yrs age group and 8% were more than 60 yrs of age. Prevalence of LSTV was higher in females when compared to males in the 40-60 and >60 age group, whereas a higher prevalence in males was noted in the 20-40 age group (Figure 1).
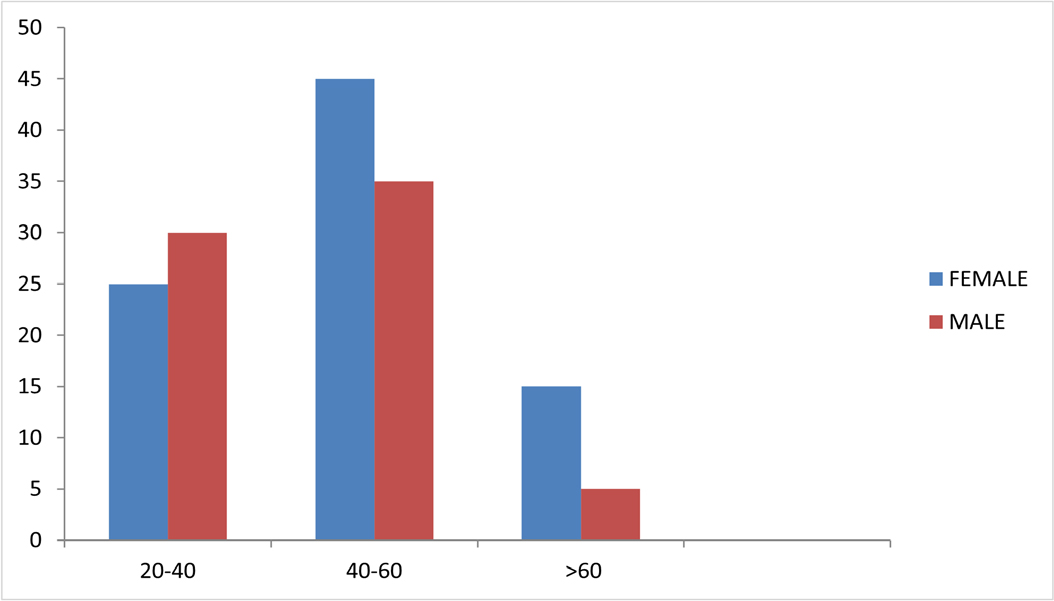
Figure 1:
Prevalence of LSTV in different age groups.
According to the Castellvi system, 24 (15.5%) patients had type I, 88 (56.7%) showed type II, 18 (11.6%) had type III and 25 (16.1%) showed type IV. Out of these patients, type IA was observed in 13.1% (Figure 2) and type IB in 2.5%. Maximum exhibited Castellvi type II in which 22.2% showed Castellvi type IIA (Figure 3) and 34.5% belonged to type IIB (Figure 4). Among Castellvi type III, 6.4% exhibited type IIIA (Figure 5), 5.2% type IIIB (Figure 6) and 16.1% showed Castellvi type IV (Figure 7and Table 2).
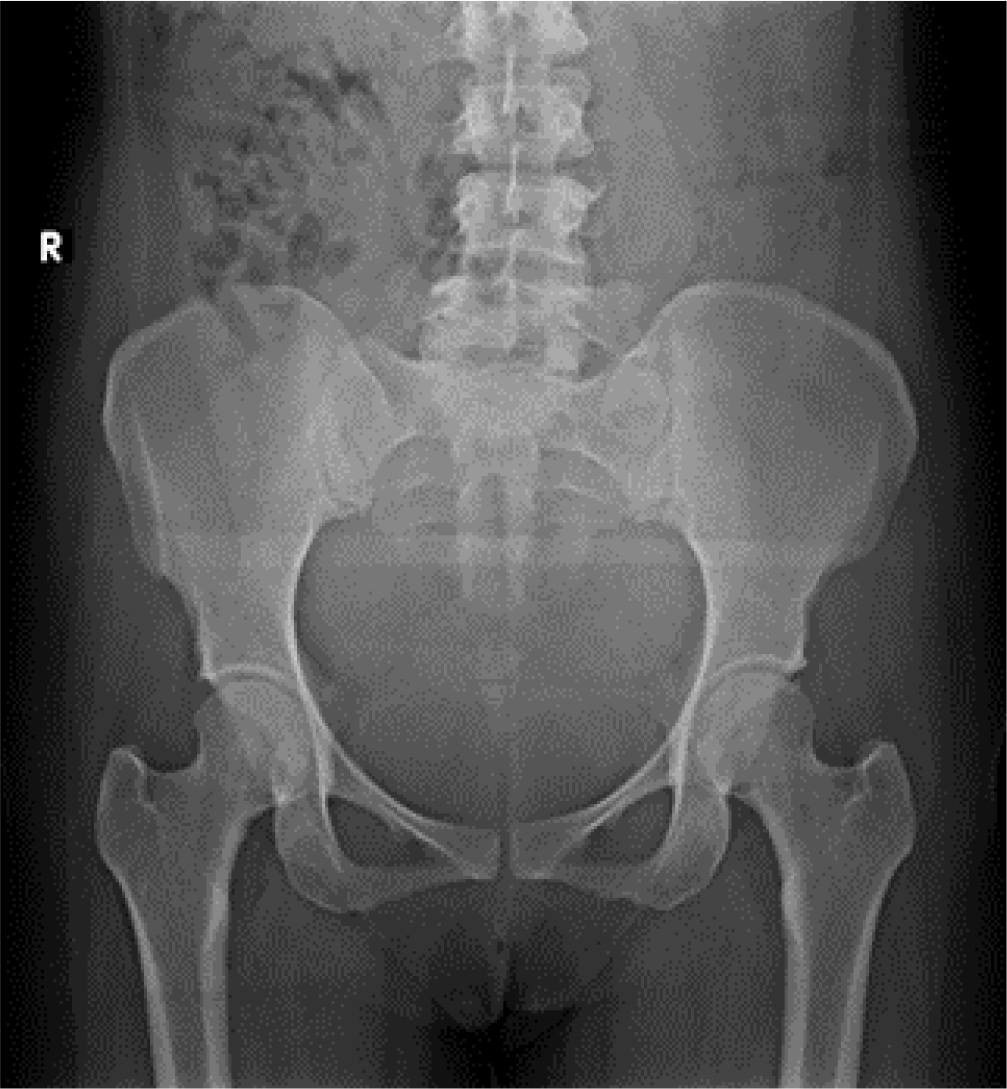
Figure 2:
Dysplastic Left L5 transverse process – LSTV type IA.

Figure 3:
Psudoarticulation of Right L5 transverse process – LSTV type II A.

Figure 4:
Psudoarticulation of bilateral L5 transverse process – LSTV type II B.

Figure 5:
True articulation of right L5 transverse process – LSTV type III A.

Figure 6:
True articulation of right L5 transverse process – LSTV type III B.

Figure 7:
True articulation of left L5 transverse process and Psudoarticulation of right L5 transverse process – LSTV type IV.
| Type | Frequency | Castellvi Type | Percentage (%) |
|---|---|---|---|
| I | 24 | I A | 13.1 |
| I B | 2.5 | ||
| II | 88 | II A | 22.2 |
| II B | 34.5 | ||
| III | 18 | III A | 6.4 |
| III B | 5.2 | ||
| IV | 25 | IV | 16.1 |
DISCUSSION
The association between an LSTV and low back pain known as Bertolotti’s syndrome, is a controversial subject which has been both supported and disputed since it was first described in 1917. Varying etiologies are thought to be the cause of low back pain in this syndrome which were seen successively emerging from various locations. The association of LSTV with the enhanced prevalence of low back pain may be due to the overwhelming effect of other spinal disorders.15 In the present study, the overall incidence of LSTV was 15.5% which was in agreement with the study of Tang et al.16 The incidence was higher in females when compared to males in the older age group which could be due to the slow decline in the protective effect of estrogen in females with advancing age. The majority of the patients showed Castellvi type II which is supported by the findings of Jeffrey et al.17 However Shaikh et al.18 indicated the presence of transitional vertebrae with both type II as well as type III. Recent findings highlighted a similar association of LSTV with type IIA and type IIB in the European population which was significantly correlated with low back pain.19 This could be due to the fact that type II LSTV showed profound effects in advancing transitional and adjacent disc degeneration.20
Interestingly, the association between LBP and LSTV subgroups demonstrates that LSTV types II and IV are affiliated with the presence of pain, as well as pain severity and frequency. However, most of the studies that support the link of LSTV with LBP with decreased physical activity implicate Castelli types II and IV.13,9 Our results differ from those of Tini et al,3 which did not demonstrate any evidence of an association of LSTV with LBP when using a subtype-specific analysis. Castellvi et al.12 stated that Type I was just a form of LSTV and not clinically relevant. Even though few studies exist linking the severity of pain to physical activity concerning LSTV, Taskaynatan et al.21 showed a significant correlation between LSTV and pain severity. The cause for the pain is the birth defect in the spine due to the abnormal bonding of the sacrum with the vertebra above due to which an additional joint is forged between the ala of the sacrum and the elongated transverse process of the vertebra above on one or both sides. This results in modification of the rotation movement of the lower part of the spine which in turn generates the back pain.22
In most of the literature, the implicated types are Castellvi II-IV. However, Aihara et al.23,8 determined that short and broad iliolumbar ligaments might have a shielding effect on the L5-S1 disk space and possibly cause destabilization at the L4-L5 level. A possible correlation may exist between the broadened long transverse processes with iliolumbar ligament morphology. Normal biomechanics of the lumbar spine is likely to be affected by transitional vertebrae.7
Patients having intense pain are likely to seek professional health care, encompassing doctor visits, drugs and surgery. Hence the association is clinically relevant. The pain was less frequent in type I, which may be suggestive of type I being a shielding factor for both LBP and buttock pain. This could be a result of an alteration of the spine movement due to a large transverse process. The proposed pathophysiological mechanisms of pain associated with LSTV types II and IV includes extraforaminal stenosis, disk prolapses, and spinal stenosis. Buttock pain that is associated with LSTV in types II and IV may result due to compression of the nerve.
The increased prevalence of LBP is associated with the presence of LSTV. Types II had the strongest correlation, which could have been caused by the pseudo articulation of the transverse process of L5 alongside the sacrum. Also, protrusion of the disc was observed more at L3/L4 and L4/L5 in type II along with enhanced occurrence of type 1 Modic changes.24
Consistent elevation in intensity and recurrence of LBP was observed in type II within the study population. Interestingly, the correlation between LBP and LSTV subgroups demonstrates that LSTV types II followed by type IV are affiliated with the presence of pain severity and frequency. The decreased frequency of pain observed in patients with LSTV type I and type III could have been the shielding factor for low back as well as buttock pain. Our study findings indicate the significance of accurately detecting the cause of LSTV because of its association with back pain. In any case of low back ache, LSTV should be considered as a differential diagnosis, specifically when the pain has been persistent with the regular mode of treatment.
Limitation
Due to poor image quality or over-projection of bowel structures, identification of patients with LSTV was occasionally difficult. The scope of this study was further limited by the rarity of this condition and the nature of the population.
CONCLUSION
Our study findings indicate the association of LSTV type II with low back pain. LSTV must be considered as part of the differential diagnosis for back pain, especially when the pain has been refractory to the conventional mode of management.
References
- Almeida DB, Mattei TA, Sória MG, Prandini MN, Leal AG, Milano JB, et al. Transitional lumbosacral vertebrae and low back pain: diagnostic pitfalls and management of Bertolotti’s syndrome. Arq Neuro Psiquiatr. 2009;67(2A):268-72. [PubMed] | [CrossRef] | [Google Scholar]
- Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol. 2004;59(11):984-91. [PubMed] | [CrossRef] | [Google Scholar]
- Tini PG, Wieser C, Zinn WM. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil. 1977;16(3):180-5. [PubMed] | [CrossRef] | [Google Scholar]
- Santavirta S, Tallroth K, Ylinen P, Suoranta H. Surgical treatment of Bertolotti’s syndrome. Follow up of 16 patients. Arch Orthop Trauma Surg. 1993;112(2):82-7. [PubMed] | [CrossRef] | [Google Scholar]
- Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006;88(9):1183-6. [PubMed] | [CrossRef] | [Google Scholar]
- Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, Moriya H, et al. Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: a clinical and anatomical study. J Bone Joint Surg Br. 2005;87(5):687-91. [PubMed] | [CrossRef] | [Google Scholar]
- Mahato NK. Lumbosacral transitional vertebrae: variations in low back structure, biomechanics, and stress patterns. J Chiropr Med. 2012;11(2):134-5. [PubMed] | [CrossRef] | [Google Scholar]
- Paik NC, Lim CS, Jang HS. Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine. 2013;38(10):E573-8. [PubMed] | [CrossRef] | [Google Scholar]
- [PubMed] | [CrossRef] | [Google Scholar]
- Konin GP, Walz DM. AJNR Am J Neuroradiol. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. 2010;31(10):1778-86. [PubMed] | [CrossRef] | [Google Scholar]
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363-70. [PubMed] | [CrossRef] | [Google Scholar]
- Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine. 1984;9(5):493-95. [PubMed] | [CrossRef] | [Google Scholar]
- Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology. 2012;265(2):497-503. [PubMed] | [CrossRef] | [Google Scholar]
- Bahadir Ulger FE, Illeez OG. The effect of Lumbosacral Transitional Vertebrae (LSTV) on paraspinal muscle volume in patients with low back pain. Acad Radiol. 2020;27(7):944-50. [PubMed] | [CrossRef] | [Google Scholar]
- Gopalan B, Yerramshetty JS. Lumbosacral transitional vertebra-related low back pain: resolving the controversy. Asian Spine J. 2018;12(3):407-15. [CrossRef] | [Google Scholar]
- Tang M, Yang XF, Yang SW, Han P, Ma YM, Yu H, et al. Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol. 2014;83(9):1679-82. [PubMed] | [CrossRef] | [Google Scholar]
- Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg. 2015;9:42 [PubMed] | [CrossRef] | [Google Scholar]
- Shaikh A, Khan SA, Hussain M, Soomro S, Adel H, Adil SO, et al. Prevalence of lumbosacral transitional vertebra in individuals with low back pain: evaluation using plain radiography and magnetic resonance imaging. Asian Spine J. 2017;11(6):892-7. [PubMed] | [CrossRef] | [Google Scholar]
- Vinha A, Bártolo J, Lemos C, Cordeiro F, Rodrigues-Pinto R. Lumbosacral transitional vertebrae: prevalence in a southern European population and its association with low back pain. Eur Spine J.. 2022;31(12):3647-53. [PubMed] | [CrossRef] | [Google Scholar]
- Cheng L, Jiang C, Huang J, Jin J, Guan M, Wang Y, et al. Lumbosacral transitional vertebra contributed to lumbar spine degeneration: an MR study of clinical patients. J Clin Med. 2022;11(9):2339 [PubMed] | [CrossRef] | [Google Scholar]
- Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, Kalyon TA, et al. Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine. 2005;30(8):E210-3. [PubMed] | [CrossRef] | [Google Scholar]
- Sharma A, Kumar A, Kapila A. Co-existence of spina bifida occulta and lumbosacral transitional vertebra in patients presenting with lower back pain. Reumatologia. 2022;60(1):70-5. [CrossRef] | [Google Scholar]
- Aihara T, Takahashi K, Ono Y, Moriya H. Does the morphology of the iliolumbar ligament affect lumbosacral disc degeneration?. Spine. 2002;27(14):1499-503. [PubMed] | [CrossRef] | [Google Scholar]
- Hanhivaara J, Määttä JH, Karppinen J, Niinimäki J, Nevalainen MT. The association of lumbosacral transitional vertebrae with low back pain and lumbar degenerative findings in MRI: a large cohort study. Spine. 2022;47(2):153-62. [PubMed] | [CrossRef] | [Google Scholar]
