ABSTRACT
Background
In hospitalized patients who are elderly and frequently have multiple comorbidities, anemia is very prevalent. The two types of anemia that are most common are iron deficiency anemia and chronic illness anemia. To assess the frequency and causes of different types of anemia in hospitalized patients using a diagnostic parameter.
Materials and Methods
According to the inclusion and exclusion parameters, a total of 111 patients were enrolled. Information was gathered from the patient’s medical documents after they were examined. Statistical analysis was done.
Results
Anemia was most frequently seen in people between the ages of 31 and 45, with 22.03% of men and 40.38% of women, and a mean age of 37.24. years. Of these, 56.75% had anemia of mild severity. It was also found that patients with chronic kidney disease and iron deficiency are the most common causes of anemia, respectively. Anemia due to chronic disease was more prevalent (30.63%), followed by iron deficiency anemia in 27.92%. Malaise (48.64%) and pallor (36.03%) were the most prevalent symptoms and signs, respectively.
Conclusion
In hospitalized patients, anemia played a significant role in deciding mortality, morbidity, and outcomes. Early detection, haemoglobin level restoration, and maintenance in these individuals may have a substantial impact on the clinical improvement of various pathological conditions.
INTRODUCTION
Anemia is a condition where the amount of red blood cells, their hemoglobin concentration, or their ability to transport oxygen are all reduced. As a result, the oxygen carrying ability is insufficient to support the physiological needs of the body.1 The individual experiences weakness, exhaustion, and shortness of breath as a result.2 There are different types of anemias each having its own cause. Some of the causes of anemia include iron or vitamin deficiency, acute or chronic blood loss, presence of a chronic illness, a genetic or acquired defect or disease or the effect of a medication. Approximately one-quarter of the world’s population, or more than one billion people, are anemic.3 More than 2 million people globally were affected in developing nations. In 2010, 32.9% of the world’s inhabitants had anemia. This percentage in confined patients can range from 40% to 50%. Depending on the person’s age, gender, and underlying cause, anemia can vary.
It is linked to a rise in hospitalized patients’ mortality rates.4 It happens when your body doesn’t have enough iron because iron is essential for the creation of hemoglobin. For your blood to transport oxygen, hemoglobin is essential. Iron deficiency anemia is a disease that results from a person not consuming enough iron, which causes their body’s iron levels to drop. One experiences severe fatigue, weakness, anorexia, vertigo, and pale skin as a consequence.5 Megaloblastic anemia is characterized by defective nuclear maturation as a result of impaired Deoxyribonucleic Acid (DNA) synthesis. There is increased cytoplasmic mass and maturation due to continued Ribonucleic Acid (RNA) synthesis. Megaloblastic anemia is caused by Vitamin B12 and folic acid deficiencies. Vitamin B12 and folate have interdependent roles in nucleic acid synthesis; therefore, deficiencies of either vitamin can cause megaloblastic anemia6 A collection of genetic disorders in which patients share a defining point mutation of the beta globin gene, sickle cell disease is also characterized by extraordinary variability of the clinical expression.7 Low RBC counts brought on by ongoing diseases are referred to as anemia of chronic disease. Cancer, Chronic Kidney Disease (CKD), and autoimmune diseases all increase the risk of getting this anemia. Obesity, Heart Failure (HF), Rheumatoid Arthritis (RA) and Systemic lupus erythematosus.8 It is a typical case of normocytic, normochromic anemia brought on by systemic inflammation, which raises the amount of hepcidin and causes the body to use iron incorrectly. It is generally a chronic illness or infection that causes anemia of inflammation. Although the exact cause is unknown, it is related to effects of chronic inflammatory diseases and infections on RBCs (chronic infections like Tuberculosis (TB), diseases with inflammation like Inflammatory Bowel Disease (IBD), RA, and Cancers like lung and breast cancer).9 When RBC cells from bone marrow are destroyed more quickly than they are produced, it is known as hemolytic anemia.10 Patients who are admitted for a variety of illnesses may already have anemia or develop it during their stay. The study’s objectives included identifying patterns and the causes of anemia, as well as the most frequently affected age groups and therapy options for hospitalized patients.
MATERIALS AND METHODS
At the Dhiraj General Hospital in Vadodara’s Department of General Medicine, cross-sectional observational research was carried out. The Sumandeep Vidyapeeth Institutional Ethics Committee (SVIEC NO: SVIEC/ ON/Phar/BNPG18/D19037) gave its ethical clearance before it could be started. The six-month research had a duration of its own (December 2021 to May 2022). It was a study aimed at examining the prevalence of different kinds of anemia with known etiologies as well as its diagnostic criteria. A total of 111 patients of either gender, older than 18 years, with hemoglobin levels below 10 g% for females and below 12 g% for males, as well as those with persistent illnesses, were included in the study (Chronic liver disease, chronic kidney disease, chronic obstructive pulmonary disease, heart failure). Pregnant women with abnormal menstrual cycles, patients who had recently lost a lot of blood, and patients who refused to give their consent were all excluded from the research. Under the direction of a biostatistician from the Dhiraj Hospital in Vadodara, the sample number was determined while considering finite population. Patients received the patient information sheet before enrolling in the research, and written informed consent was obtained. Patients provided all sociodemographic and clinical data, including their gender, age, diagnoses, and medications given, with the understanding that all data and records would be kept private. All of the collected data were entered into Microsoft Excel, where they were cleaned by cross-verifying them with the source data and correcting any out-of-range or incorrect numbers. Excel was used to complete the descriptive study.
RESULTS
A total of 111 patients from the Dhiraj hospital’s general medicine ward participated in the research. Patients range in age from 18 to >60 years, with the bulk of patients (30.63%) falling in the age group of 31 to 45 years, with a mean age of (37.24 + 5.170) (mean age + SD). Male patients outnumbered female patients (46.84%) in terms of prevalence (53.1%). By dividing the patients into groups according to the type of anemia they had, it was found that chronic disease anemia had the highest prevalence (30.63%), with patients with chronic kidney disease being particularly evident. This was followed by iron deficiency anemia (27.92%), indicating that these two conditions were the most common causes of anemia as shown in Table 1 and Figure 1. Additionally, when assessing severity, mild anemia was present in (25.22%) of patients, followed by anemia of intermediate severity in (56.75%) of patients. (See Table 1 and Figure 2). Pallor, malaise, body ache, and weakness were the most frequently noted signs and symptoms in anemic patients, with 36.03% and 48.64% respectively, when anemia was diagnosed based on clinical and laboratory results. While in this research it was found that patients with normocytic normochromic peripheral smear were highly prevalent (44.14%), followed by patients with microcytic hypochromic anemia in 40.54% of cases, Peripheral Smear (PS), Mean Corpuscular Volume (MCV), and Reticulocyte Count (RC) were included as diagnostic parameters in the laboratory findings. When MCV and RC were assessed, it was discovered that plurality of patient’s 49.54% had MCVs in the range of 79 to 91, and the remaining 49.54% had RCs below 0 [Shown in Table 2 and Figure 2].
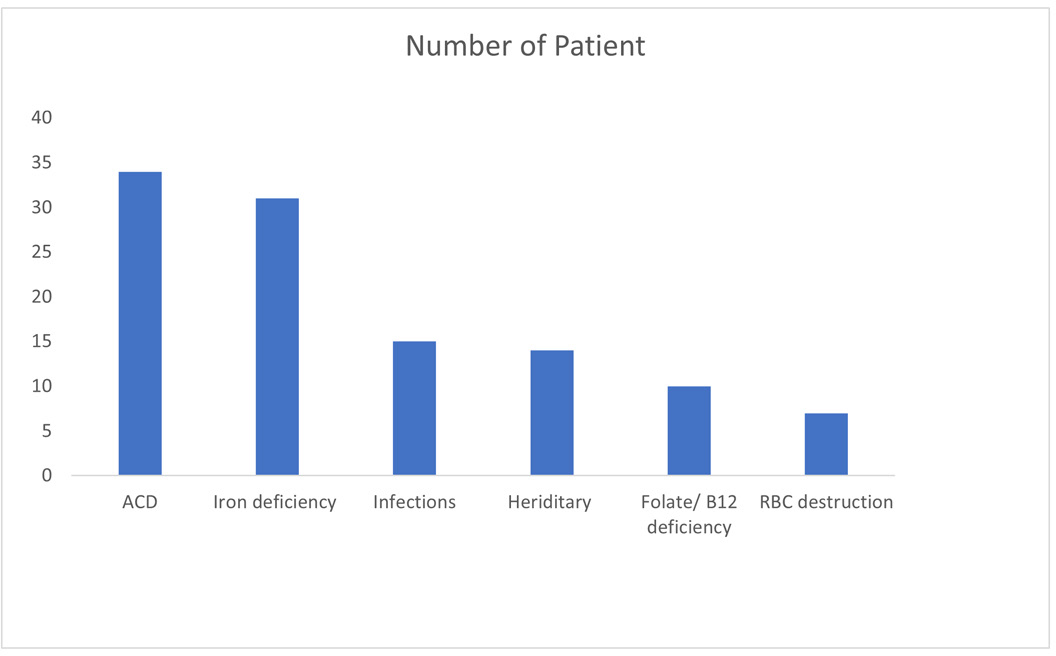
Figure 1:
Number of patients based on etiology.

Figure 2:
Number of patients based on severity.
| Parameters | Number of Patients | Prevalence (%) | ||||
|---|---|---|---|---|---|---|
| Age Group | Male | Female | Male | Female | ||
| 18- 30 years | 31 | 19 | 12 | 27.92 | 32.20 | 23.07 |
| 31-45 years | 34 | 13 | 21 | 30.63 | 22.03 | 40.38 |
| 45- 60 years | 25 | 11 | 14 | 22.52 | 18.64 | 26.92 |
| >60 years | 21 | 16 | 05 | 18.91 | 27.11 | 9.61 |
| Gender | ||||||
| Male | 59 | 53.1 | ||||
| Female | 52 | 46.84 | ||||
| Severity of Anemia | Male | Female | Male | Female | ||
| Mild | 28 | 08 | 20 | 13.55 | 38.46 | |
| Moderate | 63 | 37 | 26 | 62.71 | 50.00 | |
| Severe | 20 | 14 | 06 | 23.72 | 11.53 | |
| Parameters | Number of Patients | Prevalence (%) | |||
|---|---|---|---|---|---|
| Types of Anemia | |||||
| Anemia of chronic disease | 34 | 30.63 | |||
| Iron deficiency anemia | 31 | 27.92 | |||
| Anemia of infection/ inflammation | 15 | 13.51 | |||
| Sickle cell anemia | 14 | 12.61 | |||
| Megaloblastic anemia | 10 | 9.00 | |||
| Hemolytic anemia | 07 | 6.30 | |||
| Etiology | |||||
| Chronic diseases | CKD | 34 | 18 | 30.63 | 52.94 |
| CLD | 07 | 20.58 | |||
| HF | 06 | 17.64 | |||
| COPD | 03 | 8.82 | |||
| Iron deficiency | 31 | 27.92 | |||
| Infections | 15 | 13.51 | |||
| Hereditary | 14 | 12.61 | |||
| Folate/ Vitamin B12 deficiency | 10 | 9.00 | |||
| RBC destruction | 07 | 6.30 | |||
| Clinical Presentation | |||||
| Signs | Pallor | 40 | 57.97 | ||
|
Symptoms |
Icterus | 08 | 11.59 | ||
| Edema | 21 | 30.43 | |||
| Total | 69 | 100 | |||
| Malaise/ weakness | 54 | 48.64 | |||
| Breathlessness | 25 | 22.52 | |||
| Chest pain | 13 | 11.71 | |||
| Decreased urine output | 13 | 11.71 | |||
| Hematemia | 03 | 2.70 | |||
| Melena | 03 | 2.70 | |||
| Laboratory Investigation | |||||
| MCV | <79 | 45 | 40.54 | ||
| 79-91 | 56 | 50.45 | |||
| >91 | 10 | 9.00 | |||
| RC | <0.5 | 55 | 49.54 | ||
| 0.5- 1.5 | 49 | 44.11 | |||
| >1.5 | 07 | 6.30 | |||
| PS | Normocytic | 49 | 44.14 | ||
| Microcytic | 45 | 40.54 | |||
| Macrocytic | 10 | 9.00 | |||
| Target cells | 07 | 6.30 | |||
DISCUSSION
The current research included a total of 111 patients who were hospitalized and discovered to be anemic. In the current research, the mean patient age was roughly 31% in the age range of 31-45 years, followed by 28% in the 18-30 years. Only 18% of people were over 60. a research project Chi Huu Hong Le carried out in the USA in November 2016. They also discovered that only 8530 cases, or 18% of the 41026 total, were over the age of 60. Comparing the two studies, it was found that anemia was most prevalent in people between the ages of 31 and 45. However, the same research found that anemia was most prevalent in people aged 15 to 29. In the current research, it was discovered that a small male preponderance (53.1% versus 46.9%) and anemia prevalence that was almost equal in males and females. Male and female anemia prevalence was nearly equal in the research mentioned above. The male population exhibits a greater prevalence of occurrence (50.50% versus 49.49%) when compared to a study of a comparable nature. Both investigations reveal the same findings, namely that anemia occurs more frequently in men than in women.11 More than half of the patients (56.75%) had intermediate severity anemia, according to the distribution of patients based on anemia severity. Figure 2 illustrates that only 18% of the individuals had severe anemia. In a related study published in July 2013 by Colleen G. Koch et al., the researchers found that 30% of patients had severe anemia, compared to 41% of patients with mild anemia.12 Regarding the prevalence of different types of anemia, the study revealed that, as shown in Figure 1, 30.63% of patients had chronic disease-related anemia, (27.92%) had iron deficiency anemia, (13.51%) had an infection-or inflammation-related anemia, (12.61%) had sickle cell anemia, (9.0%) had megaloblastic anemia, and (6.30%) had hemolytic anemia. Iron deficiency anemia and persistent disease-related anemia nearly coexisted (One third patients). In research done in March 2020 by Maria Lugia Randi et al. The most prevalent type of anemia in the general population was iron deficiency anemia, but in hospitalized patients, the prevalence of this type of anemia dropped and rose for other types of anemia. In hospitalized patients, anemia of chronic disease, one of the forms of hypoproliferative anemia, is just as common as iron deficiency anemia. In this study, it was found that chronic inflammatory diseases were the primary cause of anemia in the majority of patients (36.03%), followed by iron deficiency (27.92%) and infections (13.51%). These diseases included Chronic Kidney Disease (CKD), liver disease, Chronic Obstructive Pulmonary Disease (COPD), and heart failure. Similar research by Maria Luigia Randi, et al. in Italy in 2020 came to the conclusion that chronic inflammatory diseases, followed by iron and B12 deficiency and folate deficiency, were the most prevalent causes of anemia in patients.13 Palor, which was present in one-third of patients (36%) and icterus, which was present in 18% of patients, was the most prevalent symptom in the research. In research published during December 2013 in India by Ratre BK, et al., they also came to the conclusion that pallor was the most typical symptom. In this research, we discovered that weakness and fatigue, which were present in 45% of patients, were the most frequent presenting symptoms in almost half of the patients. According to research conducted by Ratre BK et al. in December 2013, breathlessness is the second most typical symptom, followed by weakness and fatigue. Breathlessness was the second most prevalent symptom in this research, which was present in 25% of patients, behind only minor percentages of pedal edema, chest pain, and melena.14 According to research findings, patients with megaloblastic anemia had high MCV levels (>91), whereas those with Iron Deficiency Anemia (IDA), sickle cell anemia, had low MCV levels (79). According to research by Sirisha Kundrapu et al. published in 2017 in the USA, patients were diagnosed with microcytic hypochromic anemia when their MCV levels were low, normocytic normochromic anemia when their MCV levels were normal, and megaloblastic anemia when their MCV levels were high. In the present study it was observed that patients diagnosed with IDA, sickle cell anemia, and megaloblastic anemia had low RC value and in hemolytic anemia, high RC levels were observed. In a similar study conducted by Sirisha Kundrapu, et al. in 2017, the USA concluded that RC can help in the diagnosis of different types of anemia. High RC can occur due to increased erythropoietin EPO which is seen in hemolytic anemia and low RC can occur due to decreased production of RBC or decreased EPO levels as seen in IDA, megaloblastic anemia. In the present study, it was observed that hemolytic anemia was characterized by high RC levels, whereas patients with IDA, sickle cell disease, and megaloblastic anemia had low RC values. According to related study by Sirisha Kundrapu, et al. that was published in 2017, the USA came to the conclusion that RC can help with the diagnosis of different anemia types. Low RC can be caused by reduced RBC synthesis or low EPO levels, as seen in IDA and megaloblastic anemia, and high RC can be caused by excessive EPO levels, as seen in hemolytic anemia.15 The majority of the patients in the current research had microcytic hypochromic anemia (40.54%), which was followed by normocytic normochromic anemia (44.14%), while smaller percentages of patients had macrocytic and fragmented cells (9.0% and 6.30%), respectively. In 2012 research by Chanchal Das et al., India found that normocytic normochromic anemia was present in 51.6% of participants, followed by microcytic anemia (43.3%). In the current study, it was discovered that the majority of the patients under investigation had microcytic hypochromic anemia (40.54%), followed by normocytic normochromic anemia (44.14%), while smaller percentages of patients had macrocytic and fragmented cells (9.0% and 6.30%).16
CONCLUSION
The research revealed that the majority of anemia diagnoses occurred in patients between the ages of 31 and 45 who were predominantly male and who had a moderate form of anemia. Chronic illnesses were the most typical source of anemia in hospitalized patients. Where it was found that patients with chronic kidney illness were more frequently seen. From the result the conclusion was drawn that the iron deficiency anemia was the second most common form of anemia after chronic disease anemia, which was more common in the female population.
References
- McLean E, Cogswell M, Egli I, Wojdyla D, De Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993-2005. Public Health Nutr.. 2009;12(4):444-54. [PubMed] | [CrossRef] | [Google Scholar]
- Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Am J Hematol. 2014;123(5):615-24. [PubMed] | [CrossRef] | [Google Scholar]
- Ludwig H, Strasser K. Symptomatology of anemia. Semin Oncol. 2001;28(2-S8):7-14. [PubMed] | [CrossRef] | [Google Scholar]
- Klee GG. Cobalamin and folate evaluation: measurement of methylmalonic acid and homocysteine vs vitamin B12 and folate. Clin Chem. 2000;46(8 Pt 2):1277-83. [PubMed] | [CrossRef] | [Google Scholar]
- Serjeant GR, Vichinsky E. Variability of homozygous sickle cell disease: the role of alpha and beta globin chain variation and other factors. Blood Cells Mol Dis. 2018;70:66-77. [PubMed] | [CrossRef] | [Google Scholar]
- Weinstein DA, Roy CN, Fleming MD, Loda MF, Wolfsdorf JI, Andrews NC, et al. Inappropriate expression of hepcidin is associated with iron refractory anemia: implications for the anemia of chronic disease. Blood. 2002;100(10):3776-81. [PubMed] | [CrossRef] | [Google Scholar]
- Dallalio G, Fleury T, Means RT. Serum hepcidin in clinical specimens. Br J Haematol.. 2003;122(6):996-1000. [PubMed] | [CrossRef] | [Google Scholar]
- Liew CF, Cheah JS. Hereditary spherocytosis, a pitfall in the assessment of glycaemic control. Singapore Med J. 2003;44(2):94-7. [PubMed] | [Google Scholar]
- Le CH. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003-2012). PLOS ONE. 2016;11(11):e0166635 [PubMed] | [CrossRef] | [Google Scholar]
- Koch CG, Li L, Sun Z, Hixson ED, Tang A, Phillips SC, et al. Hospital‐acquired anemia: prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-12. [PubMed] | [CrossRef] | [Google Scholar]
- Skikne BS, Punnonen K, Caldron PH, Bennett MT, Rehu M, Gasior GH, et al. Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: a prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am J Hematol. 2011;86(11):923-7. [PubMed] | [CrossRef] | [Google Scholar]
- Ratre DBK, Patel DNP, Patel DU, Jain DR, Sharma DVK. Clinical and epidemiological profile of anemia in central India. Int J Med Res Rev.. 2014;2(1):45-52. [CrossRef] | [Google Scholar]
- Randi ML, Bertozzi I, Santarossa C, Cosi E, Lucente F, Bogoni G, et al. Prevalence and causes of anemia in hospitalized patients: impact on diseases outcome. J Clin Med. 2020;9(4):950 [PubMed] | [CrossRef] | [Google Scholar]
- Das C, Sahana PK, Sengupta N, Giri D, Roy M, Mukhopadhyay P, et al. Etiology of anemia in primary hypothyroid subjects in a tertiary care center in Eastern India. Indian J Endocrinol Metab. 2012;16(S2):S361-3. [PubMed] | [CrossRef] | [Google Scholar]
