ABSTRACT
Health management information system (HMIS), is a system for recording, storing, retrieving, and analyzing health data in order to make better decisions concerning delivery of health-related services. The purpose of this review article is to understand how HMIS can be used to design health-care delivery using advanced, ingenious, and revolutionary technologies such as Artificial Intelligence (AI), Innovative Digital Technologies (IoT), and Big Data, among others. Technology pervades every aspect of our lives, from phones to automobiles to healthcare and medicine. HMIS covers mHealth and e-Health cards. The review covers a range of big data areas that have been useful in establishing HMIS. It also includes anticipated opportunities and benefits, as well as some incredible obstacles. In this article there is a description of some of the responsibilities played by HMIS amid the pandemic’s crisis.
INTRODUCTION
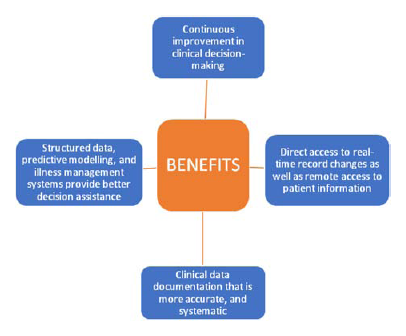
Information technology has established itself in a multitude of sectors, and the advantages of digitalization are now widely understood in the field of pharmaceuticals, medical devices, diagnostics etc. and are termed as health information system (HIS) in medical and allied fields.1 Health information system is a database management system for healthcare information. It is used to manage data pertaining to health organizations.2 Healthcare practitioners, governmental clinics, and hospitals have access to HIS and can use it for analyzing delivery of services and taking appropriate decisions accordingly.3 Everyone in healthcare, from patients to clinicians to public health officials, can benefit from the health information system. Both the central and state governments gather information related to health, thus the central and state agencies are the primary sources of health information.4 Health and associated information sources have been divided into two categories as shown in Figure 1.
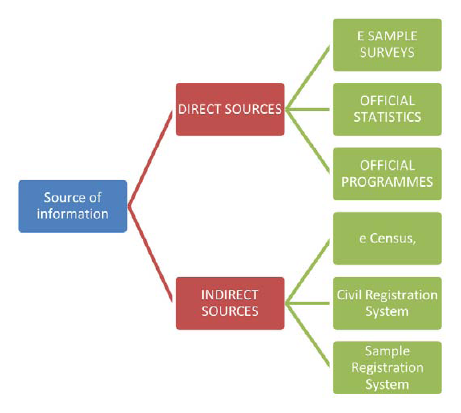
Figure 1.
Sources of information associated to health.
In today’s world, where pandemics like COVID are becoming more frequent, digitalization and computerization of health services and information have become essential in all fields. This review article focuses on the development of healthcare services with innovative digital technologies, initiatives of HMIS in Delhi-NCR and highlights the challenges and opportunities in this segment. It is organized into segments as follows: Segment 1 explains how the HMIS has progressed from paper-based records to modern technologies including E-computing, E-records, and future prospects. Segment 2 presents (MoHFW) Ministry of Health and Family Welfare programmes, eHealth and mHealth system development in other countries, such as District Health Information Software (DHIS),1 OpenMRS,2 Open ELIS, Baobab Health Trust,3 and Smart care in America, Asia, and Africa. Also emphasise the implementation strategy of HMIS and the E-card system in Delhi-NCR by the state and central government to improve healthcare infrastructure. Segment 3 draws attention to the importance of various technologies such as big data, AI, cloud or mobile computing etc. The majority of these tools are web-based and are used to simplify difficult processes and improve HMIS deployment.5 Segment 4 describes the opportunities and benefits of HMIS to improve healthcare, cost, medical records, and predict ADR.Segment 5 shows how the HMIS deals with pandemic situations. During the pandemic, HMIS played a critical role. For example, HMIS created easy survey evaluations by using technologies such as AI, data analytics, etc. Finally, Segment 6 discusses the challenges and roadblocks that will be encountered along the way. Technology, as we all know, is a blessing for our future healthcare. However, it may pose certain bad repercussions, such as concerns about secrecy and privacy. Apart from that, we need to improve our HMIS facility in order to provide better healthcare.
Evolution of Innovative Technologies in HMIS
Although health technology has been around for a long time, it was only implemented in the second half of the twentieth century. HIS serve multiple users and a broad range of purposes, such as information acquisition to identify issues that need addressing, make evidence-based health policy decisions, and allocate scarce resources optimally.6 In the meantime, remarkable progress has been made in medicines, informatics, tracking disease during pandemics and deploying treatments.7 There are presently no areas of health care management that are not supported by informatics, particularly those that require the most advanced IT and informatics innovations, such as electronic health records, clinical decision support systems, and health care data analytics.8 The history of use of information technology ranges from the most basic form of recording a patient’s symptoms, complaints, and treatment for the use of a single provider to a comprehensive aggregation, integration, and harmonization of data to support collaboration among providers, researchers, and administrators.9 Consolidation of these technologies resulted in HMIS and it has been demonstrated that it improves the efficiency of not only health care delivery but also health research studies. Although no crystal ball can forecast the future, it is safe to assume that as health systems grow and expand HMIS may require privacy and security experts, data analysts, health information managers, and information release experts in the future. However, experts predict that HMIS will perform those roles in vastly diverse ways and healthcare areas than it did earlier.10 The government is also taking steps to improve this system. For instance, the Delhi Government is implementing the HMIS to improve the city’s healthcare infrastructure.11 This digital transformation is altering our economy and society at a breakneck pace, affecting a wide range of industries, including health care.12 Digital health, according to the World Health Organization (WHO), is an umbrella term that encompasses e-health and sophisticated computer sciences (for example, in the disciplines of big data, genomics, and artificial intelligence). Many countries have also acknowledged the importance of digital health at a global level, committing to the WHO’s 13th General Programme of Work, which recognizes digital health as critical to achieving the objective of transforming the future of public health.12
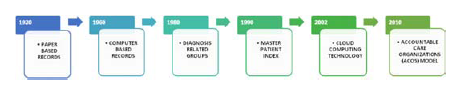
Figure 2.
The evolution of HMIS.
HMIS: An Initiative
The Ministry of Health and Family Welfare, Govt. of India has undertaken several projects to improve the efficiency and efficacy of the public healthcare system by utilizing ICT.3 One such project is the HMIS, which is a digital portal initiative of the National Health Mission, Ministry of Health and Family Welfare (MoHFW). The HMIS site is monitored in real time and supports all e-Government standards. HMIS supports Integrated Health Information Platform (IHIP) links as well as Application Programming Interface (API) integration with other programmes.2 The new real-time HMIS portal provides access to a variety of data on India’s health indices. Many developing countries have robust HIS capable of meeting a wide range of information needs.1
For instance, Brazil has embarked on an initiative to reform the health system. SIGA (São Paulo City Health Information System) offers a unique perspective on how to conceptualize revolutionary HIS.13 The Smart care system programme has been implemented in Zambia. Global eHealth, which supports the care of patients in resource-poor countries in Africa, Latin America, and Asia, has arisen over the previous decade. These include the DHIS,1 OpenMRS,2 Open ELIS, Baobab Health Trust,3 and Smartcare, which are all currently in widespread usage in many countries.13 The emergence of mobile health informatics, or “mHealth,” is also significant. In the developing world, eHealth systems are rapidly proliferating and demonstrating positive clinical and programmatic outcomes.11 The Delhi government is also expecting to implement its ambitious project of a cloud-based HMIS very soon. It would provide a single platform from which we can easily access the number of vacant beds, medicine stock, number of ventilators present, and other medical infrastructure information. They will also distribute e-health cards that contain the cardholder’s entire medical history, and the patient would be able to receive treatment at any hospital on the HMIS.11 Based on voter IDs, QR code-based cards with complete demographic and vital clinical details, as well as information regarding the individual’s eligibility under several Delhi government health plans, will be distributed. Each citizen will receive two permanent cards, one large with detailed information and the other smaller, like an ATM card. HMIS will be implemented in all government hospitals, first in government hospitals and eventually in all private hospitals, with all patient care services being brought under this system. Delhi residents will be given a health card that would entitle them to free healthcare services. QR Codes will be used to represent GIS coordinates of the patient’s current address. It will have integrated biometric and facial recognition data linked to health cards. The Delhi government is attempting to provide advanced healthcare facilities to its citizens in this manner.14
The Importance of Technology in Healthcare’s Big Data
Big data refers to vast, diversified amounts of data that are growing at an exponential rate. The volume of data, the velocity with which it is created and collected, and the variety or scope of the data points covered (known as the “three v’s” of big data) are all factors to consider. Big data is frequently derived by data mining and is available in a variety of formats.15 A large amount of data is accessible at various hospitals and healthcare institutions across the world, which is collected from disease-affected people. Unique fusion algorithms would be required to find meaning in the massive mounds of patient data as technology is integrated into healthcare. The availability of machine learning and AI technologies as part of cloud services has aided in the more accurate interpretation of enormous volumes of patient data.16 Digitization of healthcare data, advances in computer processing and data storage, has enabled the creation of complex algorithms in the form of AI.16 It
enables computer systems to do human brain activities in a variety of disciplines. It is often presented in many applications that use big data, which comprises all the important data regarding medical health and disorders that a model may access during execution or disease diagnosis. It plays a crucial part in the design of medications and the identification of adverse effects of pharmaceutical products.17 The major benefits of AI are based on its ability to continually scan the EMR, training on previous patients’ trajectories and refine the lenses of their own prescription glasses.18 The use of analytics, machine learning, and AI on big data allows for the detection of patterns and correlations, and so delivers actionable insights for enhancing healthcare delivery. The advancement of Information and Communication Technologies (ICT) has undeniably enhanced people’s lives all around the world and has resulted in a much-needed and substantial advance in the health sector, which is usually referred to as electronic health (eHealth) and medical health (mHealth). Despite the incorporation of big data processing methodologies and platforms into existing data management designs for healthcare systems, these architectures struggle to avert emergency instances.19
Using cloud solutions that include the expert system’s knowledge base, any data acquired from different devices, wearables, or trackers may be combined and evaluated. The patient and their doctors will have access to these cloud-based reports, which will be safe since they will be accessible through an appropriate authentication system. Based on the algorithms and rules contained in the knowledge base, the expert system will provide the patient with preventive measures and other health information.20 As a result of greater accuracy, care practitioners can deliver more individualized suggestions to their patients. This technique allows patients to receive high-quality care without ever having to visit a hospital.21 We can employ cloud computing to scan documents automatically and produce data sets that data scientists may use to train and construct models. Consequently, expenses are lowered, the workforce is decreased, and paperwork is minimized. Mobile Cloud Computing [MCC] is a method of combining mobile devices and cloud computing to improve the quality of information management and transfer. As a result, data management, scheduling appointments, and locating the finest physicians and neighboring health facilities becomes easier and faster.22 Cloud computing services can offer a future-proof approach to AI research and boost the chances of success throughout the healthcare industry.
Opportunities and Benefits of HMIS
Globally, health-care systems are increasing their use of electronic health records to increase access to patient data for administrative, therapeutic, and research purposes. The aim for deploying HIS in-healthcare settings is to improve quality of healthcare services. HIS are viewed as “silver bullet” solutions targeted at increasing efficiency in the healthcare system and as a result, lowering long-term healthcare costs and increasing organizational profitability.23,24 It is predicted that HIS will cut record-keeping costs while fulfilling privacy regulations. HIS is also intended to allow for automatic information exchange among physicians, minimise office visits and hospital admissions, and even lower the chance of malpractice lawsuits.25
Reduction In Medical Errors
According to the Institute of Medicine (IOM) (1999) research, up to 98,000 individuals die in U.S. hospitals each year because of avoidable medical mistakes.26 It also estimated that if current technical know-how were deployed, 50% of mistakes could be removed during a five-year period. The IOM specifically included the use of Health Information Technology (HIT), such as e-prescription, as a crucial solution aspect in their list of remedies to this problem. Clearly, the function of HIS in boosting readability and reducing medical errors in healthcare services has been demonstrated to be a potential advantage.
Improved Overall Quality of Healthcare
Predicting ADRs
Machine learning approaches are better adapted for bigger datasets, traditional post-marketing drug surveillance methods have been superseded by machine learning for the prediction of ADRs. To extract pharmacological information and forecast ADR relationships, supervised machine learning was applied. The development of ‘big healthcare data,’ which is characterised by immense volume, complexity, and velocity, has created an attractive potential for digital pharmacovigilance research.28 As a result of the scenario, many firms are turning to AI in pharmacovigilance to help manage the growing workload and make life easier. Companies benefit from AI because it automates data collection, produces rapid results, and reduces mistakes. National Language Processing (NLP), speech to text translation, and National Language Understanding (NLU) are among the technologies used to gather ADRs with increased accuracy, speed, scalability, and cost savings.29 Based on medication commonalities such as chemical structure, mechanism of action, and polypharmacy side effects, AI-based analytics can be used to anticipate previously unknown adverse drug effects.30,31 Deep learning approaches based on neural fingerprints have been found to not only predict but also identify the chemical substructures involved with bad medication responses.32 These algorithms can help in the creation of safer pharmaceuticals based on scientific data. To aid decision-making, ML may be used at the point of care to deliver tailored ADE risk estimations and treatment recommendations.33
Role of HMIS in Handling Pandemics
HIS have been crucial in reacting to the COVID-19 pandemic, not only as platforms for efficient and effective communications, but also in fundamentally changing the dynamics of relationships between healthcare practitioners and customers, as well as the delivery of healthcare services.34 The healthcare industry has been completely transformed by the digital revolution. Technologies that have had a considerable influence during pandemic in the healthcare industry are:
a) Artificial Intelligence: AI-based technologies that patients are familiar during COVID-19 are chatbots and virtual health assistants. AI chat bots play a crucial role in the healthcare business, from customer service personnel to diagnostic tools and even therapists.35 This technology is boosting healthcare services in a variety of ways, from balancing healthcare partners and partnerships to increasing healthcare personnel productivity and providing better patient care in pandemic.
b)Healthcare Big Data: Big data analysis finds preventative programmes and assists professionals in COVID-19 emergencies, making preventive care simpler. Bigdata predictive analysis is assisting hospitals and clinics in predicting future admissions, which simplifies the medical workforce’s availability for patient care and improves hospital performance.34
c)IoT in Healthcare: Prior to the introduction of IoT, individuals’ interactions with their healthcare providers were restricted to clinical visits or text or phone call exchanges. However, the IoT has reshaped this practise and enabled the idea of remote monitoring. Hospitals can track their medical equipment, such as nebulizers and oxygen pumps, using sensors included into IoT devices. They can also track the whereabouts of their medical personnel in real time, which is extremely useful in an emergency.
d)Cloud Computing: The utilisation of the cloud enables for greater operational efficiency, cost reduction, and improved patient care. Cloud infrastructure solutions let health care organisations store data more easily and get access to genuine data interoperability.
e)Data Analytics: The need for high-quality, timely data has long been a top concern in the healthcare industry, and the emergence of COVID-19 has amplified that requirement. Health organisations are rushing to create and deploy data analytics in their business operations to deal with COVID-19. Machine learning and data analytics will be crucial in detecting and tracking the progression of this disease, as well as the responses to it.36
Challenges and Barriers in implementation of HMIS
Despite the enormous potential and prospects for HIS, there are several concerns that must be addressed.37 Hospitals lack the rules and laws necessary to support IT development efforts inside their organizational structures. Many stakeholders are either hesitant to utilize the new system or entirely ignore it since there are no norms or regulations in place to make it necessary in order to promote the engagement.38,39 Many
healthcare organizations are concerned about the direct and indirect expenses of HIS. This is especially true given the expensive initial outlays and limited perceived return on investment.40,41 Reengineering business processes is likewise a demanding task.42 The majority of the changes that occur with HIS deployment necessitate significant organizational changes that necessitate not only financial expenditures but also a complete shift in how company/ organization is conducted. Finally, there is a relationship between financial and clinical results that specifies, to a degree, how much money should be spent to attain a specific health outcome. As a result, the expense of acquiring, operating, and maintaining HIS remains a significant barrier. When institutions use HIS, privacy issues and security hazards such as hacking, identity theft, and unauthorized access to medical data are seen as a big issue. This problem has a significant impact on people’s decisions and behaviours when it comes to information systems.43 As a result, system providers should make a concerted effort to invest in privacy and security protection to mitigate the impact of these hurdles and guarantee users that the information they submit or share through the system is secure. Because these worries are reasonable, investing in privacy protection and security solutions is a wise investment that institutions should recognise as a valued asset.44 However, these issues should not lead people to fully reject the usage of an electronic medical record. For the benefit of all persons in society, organisations should work on raising awareness of the need of having e-health systems and electronic medical records.45
The effective implementation of HIS initiatives necessitates the coordination of several activities at multiple levels in complicated settings.46 As a result, those in charge of implementing HIS initiatives in developing nations should consider the contextual features of the institutions, sector, and region in which they are located. Setting specifications and rules for all healthcare providers must be of high quality and satisfy the standards, which is undoubtedly more essential than transitioning to e-health. Issues of this kind are exceedingly difficult to resolve, and staff are fully aware that most of the team is doing everything they can to enlist the help of all healthcare specialists.47
Design and Development Challenges
Any feature or function of a sophisticated health IT–based clinical application can put patients, the organization in charge of their treatment, or even the system’s creators at danger.48,49 When the severity and likelihood estimations of a prospective error are combined, we should be able to generate an overall proactive risk for that error class. To comprehend the potential danger, we need new proactive, data-driven models, approaches, and tools for evaluating both the severity and frequency of these occurrences.
Data input and comprehension problems are caused by poor user interface design.50 Because of the inconsistency and absence of agreed and implemented standards, the provider is forced to swap mental models about how each interface works on a regular basis, which raises the risk of mistake.51 We need standardized methods for allowing users to submit data and automatically verifying that the data supplied is valid for a specific patient.52 Finally, for the design, development, and testing of safety-critical software, the industry must adhere to well-established standards. National or international standards bodies may establish these guidelines, which are then adopted by governments or other authorities. Regardless how extensive a single health IT vendor’s product offerings are, new health IT capabilities and stand-alone apps will always be produced that must be interfaced to the existing system (s).53 The whole development, implementation, patching, and update process should be error-free.
Implementation and use Challenges
Users of busy clinical applications will continue to make mistakes. Health IT should serve as both a cockpit and a “safety net,” making it simpler to do the right thing while also catching faults.54,55 Providing the right degree of artificial intelligence (AI)-driven automation and guaranteeing its safety and dependability, are crucial to effective health IT.56 Transitioning from an in-house built EHR to a commercial offthe-shelf EHR or from one commercial EHR to another, as well as large enhancements to an existing EHR, all pose safety issues.57
CONCLUSION
In the year 2022, the digital transformation of healthcare is quite promising. Healthcare providers are looking for a way to modernize their existing systems with novel HMIS. It allows storing, managing, and exchanging health information within and among hospitals because the healthcare industry is a heterogeneous system made up of disparate data silos with a lack of standardization. The goal is to improve patient care and productivity. And, in this case, technology aids in achieving these goals as quickly as possible. One such approach is the Delhi government’s initiative to deploy innovative HMIS and eHealth cards for the benefit of patients. In the face of a pandemic, AI, IoT, big data, cloud services, and other digital healthcare technologies are transforming the working paradigm of this industry. As a result, the patient’s interaction with health experts is improved, data is secured, informed decisions are made, and companies can provide better health solutions and more favorable outcomes. Other significant advantages include reduced medical errors, improved clinical decision-making during patient contacts, and real-time universal access to a patient’s information. However, while introducing health information technology into a complex adaptive health system has the potential to improve care, it also has unintended consequences and introduces new barriers. Assuring the safety of health information technology and its usage in clinical settings has emerged as a major challenge. To lower the frequency of harm, there are significant opportunities to improve safety by leveraging big data, AI, and other novel technologies across the health sector areas. Healthcare management is undergoing significant changes that are transforming the image of the medical industry. It is likely to improve further as technology advances.
Cite this article
Dahiya S, Goyal Y, Sharma C. Designing Delivery of Healthcare Services with Health Management Information System, AI, Big Data, and Innovative Digital Technologies. J Young Pharm. 2022;14(4):366-71.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- Brook C. [[cited Mar 27 2022]];What is a health information system? [internet]. DataInsider Digital Guardian’s Blog. 2020 Available from: [Google Scholar]
- [Array];Types of information systems used in healthcare facilities. Scott-Clark Medical. 2018 Available from: [Google Scholar]
- Pandey A, Roy N, Bhawsar R, Mishra RM. Health information system in India: Issues of data availability and quality. 2010;29(1):111-28. [Google Scholar]
- [Array];Chai W. cloud computing [internet]. 2021 Search cloud computing. Techtarget. Available from: [Google Scholar]
- Health information systems [internet]. World Health Organization. [[cited Mar 26 2022]];Toolkit on monitoring health systems strengthening. 2008 Available from: [Google Scholar]
- Haux R. Health information systems – past, present, future. Int J Med Inform. 2006;75(3-4):268-81. [PubMed] | [CrossRef] | [Google Scholar]
- Simoes E. Health information technology advances health care delivery and enhances research. Mo Med. 2015;112(1):37-40. [PubMed] | [Google Scholar]
- [[cited Mar 26 2022]];The history of health information management-from then to. Now Publishers [internet]. 2022 Open textAvailable from: [PubMed] | [Google Scholar]
- Dimick C. 2025: current ”health IT revolution” drastically changes HIM in the near future. Journal of AHIMA 83. Health Inf Manag. 2012;8:24-31. [PubMed] | [Google Scholar]
- [[cited Mar 26 2022]];Business Today. Delhi to launch cloud-based health management system in 2021 [internet]. 2021 Available from. Available from: [PubMed] | [Google Scholar]
- Negreiro M. [[cited Mar 26 2022]];The rise of digital health technologies during the pandemic. European Parliamentary Research Service [internet]. p. 1-10. 2021 Available from: [PubMed] | [Google Scholar]
- [[cited 17/8/2022]];Bill and Melinda Gates Foundation. Health information systems in developing countries [internet]. 2009:33-40. Vital Wave Consulting Available from: [PubMed] | [Google Scholar]
- Roy S. [[cited Mar 26 2022]];QR code-based health cards for all in Delhi may be reality b. Read more at. The Times of India [internet]. 2021 Available from:Available from. Available from: [PubMed] | [Google Scholar]
- [[cited Mar 27 2022]];Big Data ST [internet]. Investopedia. 2021 Available from: [PubMed] | [Google Scholar]
- Stanfill MH, Marc DT. Health information management: Implications of artificial intelligence on healthcare data and information management. Yearb Med Inform. 2019;28(1):56-64. [PubMed] | [CrossRef] | [Google Scholar]
- Basile AO, Yahi A, Tatonetti NP. Artificial intelligence for drug toxicity and safety. Trends Pharmacol Sci. 2019;40(9):624-35. [PubMed] | [CrossRef] | [Google Scholar]
- [[cited Mar 27 2022]];AI in healthcare: How it’s changing the industry [internet]. HIMSS. 2020 Available from: [PubMed] | [CrossRef] | [Google Scholar]
- Yang YC, Islam SU, Noor A, Khan S, Afsar W, Nazir S, et al. Influential usage of big data and artificial intelligence in healthcare. Comput Math Methods Med. 2021;2021:5812499 [PubMed] | [CrossRef] | [Google Scholar]
- MacRae D. [[cited Mar 27 2022]];93% of IT industry to adopt cloud tech within five years [internet]. CloudTech. 2022 Available from: [PubMed] | [CrossRef] | [Google Scholar]
- Dubey N, Sangeeta Vishwakarma. Cloud computing in healthcare, cloud computing. Ijcter. 2016;2(5) [PubMed] | [CrossRef] | [Google Scholar]
- Jemal H, Kechaou Z, Ben Ayed M, Alimi A. Cloud computing and mobile devices based system for healthcare application. IEEE International Symposium on Technology and Society (ISTAS). 2015 [PubMed] | [CrossRef] | [Google Scholar]
- Bates DW, Saria S, Ohno-Machado L, Shah A, Escobar G. Big data in health care: Using analytics to identify and manage high-risk and high-cost patients. Health Aff (Millwood). 2014;33(7):1123-31. [PubMed] | [CrossRef] | [Google Scholar]
- Chaudhry B, Wang J, Shinyi Wu, Maglione M, Mojica W, Roth E, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742-52. [PubMed] | [CrossRef] | [Google Scholar]
- Goldschmidt PG. HIT and MIS. Commun ACM. 2005;48(10):68-74. [CrossRef] | [Google Scholar]
- Singhania R, Rao D. [[cited May 28 2022]];Internet, IT and software and Domain Name Issues – India [Internet]. 2022 Available from: [CrossRef] | [Google Scholar]
- Van de Castle B, Kim J, Pedreira ML, Paiva A, Goossen W, Bates DW, et al. Information technology and patient safety in nursing practice: An international perspective. Int J Med Inform. 2004;73(7-8):607-14. [PubMed] | [CrossRef] | [Google Scholar]
- Lee CY, Chen YPP. Machine learning on adverse drug reactions for pharmacovigilance. Drug Discov Today. 2019;24(7):1332-43. [PubMed] | [CrossRef] | [Google Scholar]
- Dhembare P. [[cited Mar 27 2022]];Artificial Intelligence (AI) in Adverse Drug Reaction (ADR) collection [internet]. The Times of India. 2021 Available from: [PubMed] | [CrossRef] | [Google Scholar]
- Zitnik M, Agrawal M, Leskovec J. Modeling polypharmacy side effects with graph convolutional networks. Bioinformatics. 2018;34(13):i457-66. [PubMed] | [CrossRef] | [Google Scholar]
- Ogallo W, Kanter AS. Towards a clinical decision support system for drug allergy management: are existing drug reference terminologies sufficient for identifying substitutes and cross-reactants?. Stud Health Technol Inform. 2015;216:1088 [PubMed] | [Google Scholar]
- Dey S, Luo H, Fokoue A, Hu J, Zhang P. Predicting adverse drug reactions through interpretable deep learning framework. BMC Bioinformatics. 2018;Array(Suppl 21 Suppl):476 [PubMed] | [CrossRef] | [Google Scholar]
- Pavani A, Naushad SM, Kumar RM, Srinath M, Malempati AR, Kutala VK, et al. Artificial neural network-based pharmacogenomic algorithm for warfarin dose optimization. Pharmacogenomics. 2016;17(2):121-31. [PubMed] | [CrossRef] | [Google Scholar]
- Liu C. Health information systems amid COVID-19 outbreak: Lessons from China. Health Inf Manag. 2021;50(1-2):99-100. [PubMed] | [CrossRef] | [Google Scholar]
- Lee D, Yoon SN. Application of artificial intelligence-based technologies in the healthcare industry: Opportunities and challenges. Int J Environ Res Public Health. 2021;18(1):271 [PubMed] | [CrossRef] | [Google Scholar]
- Parashar V. [[cited Mar 27 2022]];Array. 2022 Available from: [PubMed] | [CrossRef] | [Google Scholar]
- Islam MM, Poly TN, Li YJ. Recent advancement of clinical information systems: Opportunities and challenges. Yearb Med Inform. 2018;27(1):83-90. [PubMed] | [CrossRef] | [Google Scholar]
- Jarosławski S, Saberwal G. In ehealth in India today, the nature of work, the challenges and the finances: An interview-based study. BMC Med Inform Decis Mak. 2014;14(1):1 [PubMed] | [CrossRef] | [Google Scholar]
- Halas G, Singer A, Styles C, Katz A. New conceptual model of EMR implementation in interprofessional academic family medicine clinics. Can Fam Physician. 2015;61(5):e232-9. [PubMed] | [Google Scholar]
- Anderson GF, Frogner BK, Johns RA, Reinhardt UE. Health care spending and use of information technology in OECD countries. Health Aff (Millwood). 2006;25(3):819-31. [PubMed] | [CrossRef] | [Google Scholar]
- Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med. 2009;360(15):1477-9. [PubMed] | [CrossRef] | [Google Scholar]
- Devaraj S, Kohli R. Information technology payoff in the health-care industry: A longitudinal study. J Manag Inf Syst. 2000;16(4):41-67. [CrossRef] | [Google Scholar]
- Herrick M. D, Gorman L. [[cited 17/8/2022]];Dallas, Headquarters: National Center for Policy Analysis. p. 1-24. Goodman J. Health Information Technology: Benefits and Problems [Internet]. 2010 Available from: [CrossRef] | [Google Scholar]
- Zakaria N, Mohd Yusof SA. Understanding Technology and People Issues in Hospital Information System (HIS) Adoption: Case study of a tertiary hospital in Malaysia. J Infect Public Health. 2016;9(6):774-80. [PubMed] | [CrossRef] | [Google Scholar]
- Wen HJ, Tarn JM. Privacy and security in E-healthcare information Management. Information Systems Security. 2001;10(4):1-16. [CrossRef] | [Google Scholar]
- Krishna S, Walsham G. Implementing public informationsystems in developing countries: Learning from a successstory. Inf Technol Dev. 2005;11(2):123-40. [CrossRef] | [Google Scholar]
- Ahmadian L, Dorosti N, Khajouei R, Gohari SH. Challenges of using Hospital Information Systems by nurses: Comparing academic and non-academic hospitals. Electron Physician. 2017;9(6):4625-30. [PubMed] | [CrossRef] | [Google Scholar]
- Jalghoum Y, Tahtamouni A, Khasawneh S, Al-Madadha A. Challenges to healthcare information systems development: The case of Jordan. Int J Healthc Manag. 2021;14(2):447-55. [CrossRef] | [Google Scholar]
- Amato MG, Salazar A, Hickman TT, Quist AJ, Volk LA, Wright A, et al. Computerized prescriber order entry-related patient safety reports: Analysis of 2522 medication errors. J Am Med Inform Assoc. 2017;24(2):316-22. [PubMed] | [CrossRef] | [Google Scholar]
- Howe JL, Adams KT, Hettinger AZ, Ratwani RM. Electronic health record usability issues and potential contribution to patient harm. JAMA. 2018;319(12):1276-8. [PubMed] | [CrossRef] | [Google Scholar]
- Westbrook JI, Baysari MT, Li L, Burke R, Richardson KL, Day RO, et al. The safety of electronic prescribing: Manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals. J Am Med Inform Assoc. 2013;20(6):1159-67. [PubMed] | [CrossRef] | [Google Scholar]
- Kushniruk AW, Bates DW, Bainbridge M, Househ MS, Borycki EM. National efforts to improve health information system safety in Canada, the United States of America and England. Int J Med Inform. 2013;82(5):e149-60. [PubMed] | [CrossRef] | [Google Scholar]
- Sujan MA. Managing the patient safety risks of bottom-up health information technology innovations: Recommendations for healthcare providers. BMJ Health Care Inform. 2018;25(1):7-13. [CrossRef] | [Google Scholar]
- Sinsky CA, Privitera MR. Creating a “Manageable Cockpit” for Clinicians: A Shared Responsibility. JAMA Intern Med. 2018;178(6):741-2. [PubMed] | [CrossRef] | [Google Scholar]
- Georgiou A, Lymer S, Forster M, Strachan M, Graham S, Hirst G, et al. Lessons learned from the introduction of an electronic safety net to enhance test result management in an Australian mothers’ hospital. J Am Med Inform Assoc. 2014;21(6):1104-8. [PubMed] | [CrossRef] | [Google Scholar]
- Lyell D, Coiera E. Automation bias and verification complexity: A systematic review. J Am Med Inform Assoc. 2017;24(2):423-31. [PubMed] | [CrossRef] | [Google Scholar]
- Larsen E, Fong A, Wernz C, Ratwani RM. Implications of electronic health record downtime: An analysis of patient safety event reports. J Am Med Inform Assoc. 2018;25(2):187-91. [PubMed] | [CrossRef] | [Google Scholar]