ABSTRACT
Objectives
Benign Prostate Hyperplasia (BPH) is a common condition affecting aging males, characterized by prostate enlargement and associated urinary symptoms. Despite available treatments, medication adherence remains a challenge, leading to suboptimal outcomes.
Materials and Methods
This hospital-based study recruited 90 male BPH patients and assessed medication adherence using the Morisky Medication Adherence Scale (MMAS-8) and symptom severity using the International Prostate Symptom Score (IPSS). Statistical analysis compared baseline and follow-up data using appropriate tests.
Results
Most patients were aged 51-80 years, with moderate symptoms at baseline shifting to mild symptoms at follow-up. Medication adherence significantly improved from baseline, with fewer non-adherent patients. Common symptoms included nocturia, frequency and urgency, with tamsulosin being the predominant medication.
Conclusion
Pharmaceutical care interventions led to improved medication adherence and symptom management in BPH patients. The study underscores the importance of addressing medication adherence and symptom control in BPH management. Individualized treatment approaches and lifestyle modifications are crucial for optimizing outcomes. Further research should explore effective intervention components and long-term effects on disease progression, enhancing BPH patient quality of life.
INTRODUCTION
Benign Prostate Hyperplasia (BPH) is recognized as the most prevalent non-cancerous growth affecting the prostate gland, commonly leading to urinary symptoms in males aged 50 and older (Langan, 2019; Parsonset al., 2008). This condition involves the benign enlargement of the prostate, specifically in the periurethral transition zone surrounding the urethra, characterized by the proliferation of smooth muscles and epithelial cells (McVary, 2006). The prevalence of BPH notably increases with age, with estimates ranging from 8% to 60% among individuals aged 90 years (Aaronet al., 2016; Ghaderiet al., 2024).
Lower Urinary Tract Symptoms (LUTS) associated with BPH can be categorized into irritative symptoms related to urine storage failure and obstructive symptoms resulting from bladder emptying difficulties (Kaplan, 2022). Irritative symptoms include increased frequency, urgency and nocturia, while obstructive symptoms encompass straining, weak urinary stream and incomplete bladder emptying (Roehrborn, 2010). These symptoms may arise from BPH or other conditions such as urethral stricture disease and neurogenic voiding dysfunction (Egan, 2016).
Irritative voiding symptoms, such as urgency and frequency, can also be attributed to detrusor overactivity secondary to BPH, as well as neurological disorders, malignancy and various lifestyle factors including diuretic therapy, high fluid intake and consumption of bladder irritants like caffeine and alcohol (Lerneret al., 2021; Mobleyet al., 2015). Less common manifestations of BPH include urinary retention, inability to urinate and hematuria (Carrero-Lópezet al., 2016).
Various symptom scoring systems have been developed to evaluate the severity of Benign Prostate Hyperplasia (BPH) symptoms, with the International Prostate Symptom Score (IPSS) being the most widely utilized. The IPSS, devised by the American Urological Association (AUA), consists of eight questions and provides an assessment of seven BPH symptom characteristics. Total scores generated from the IPSS categorize the severity of the disease into mild (1-7), moderate (8-19), or severe (20-35) (Barryet al., 1992; Thorakkattilet al., 2023).
Medication adherence was assessed using the Morisky Medication Adherence Scale (MMAS-8) at both baseline and follow-up. Medication adherence refers to the degree to which patients adhere to the instructions and prescriptions provided by healthcare professionals, reflecting the extent to which patients’ behavior aligns with prescribers’ recommendations. Poor adherence is a common factor contributing to treatment failure and suboptimal treatment outcomes. The MMAS-8 scale ranges from 0 to 8, with scores of 8 indicating high adherence, scores of 7 or 6 indicating moderate adherence and scores below 6 indicating low adherence (Moriskyet al., 2008).
The present study titled “Impact of Pharmaceutical Care on Medication Adherence and Symptoms Management in Benign Prostate Hyperplasia Patients: A Hospital-Based Study” addresses a critical gap in current healthcare practices concerning BPH management. Benign Prostate Hyperplasia poses significant challenges to patient well-being, with symptoms ranging from urinary frequency to incomplete bladder emptying, impacting quality of life. Despite the availability of effective treatments, poor medication adherence remains a pervasive issue, leading to suboptimal symptom control and treatment outcomes (Yeawet al., 2009). Therefore, there is a pressing need to explore innovative approaches to enhance medication adherence and symptom management in BPH patients. This study aims to evaluate the impact of pharmaceutical care interventions, provided by clinical pharmacists alongside standard physician treatment, on medication adherence and symptom severity in BPH patients. By elucidating the role of pharmaceutical care in improving treatment adherence and symptom control, this research seeks to contribute valuable insights to optimize BPH management strategies and enhance patient outcomes.
MATERIALS AND METHODS
Study Design and Patient Enrollment
This cross-sectional study was conducted at the urology department of Sri Venkateswara Institute of Medical Sciences in Tirupati after an ethical approval with No. AS/11/IEC/SVIMS/2017/dated 1/8/2024. Ninety patients diagnosed with Benign Prostatic Hyperplasia (BPH) were recruited based on predefined inclusion and exclusion criteria. The International Prostate Symptom Score Scale (IPSS) and Morisky Medication Adherence Scale (MMAS) were utilized for patient selection.
Methods
Medication adherence was assessed using the MMAS and IPSS in BPH patients. The IPSS is a self-administered questionnaire designed to swiftly evaluate BPH symptoms and their impact on quality of life. It comprises eight questions, with a total score ranging from 0 to 35, indicating the severity of symptoms. Scores of 1 to 7 are categorized as mild, 8 to 19 as moderate and 20 to 35 as severe.
Additionally, the MMAS-8, an eight-item questionnaire, was employed to measure medication adherence. It consists of seven yes/no questions, with total scores ranging from 0 to 8. Scores of 8 indicate high adherence, while scores of 7 or 6 suggest medium adherence and scores below 6 indicate low adherence. The MMAS-8 serves as a structured self-report tool for assessing medication-taking behavior.
Statistical Analysis
Continuous variables were represented by mean±SEM, while categorical variables were expressed as counts and percentages. McNemar’s test and the Wilcoxon signed-rank test were employed for within-group comparisons of baseline and follow-up data, for categorical and continuous variables, respectively. The t-test was utilized to compare adherent and non-adherent groups at baseline and follow-up, depending on the nature of the data. All statistical tests were two-sided, with significance set at p<0.05. Analysis was conducted using SPSS version 22, involving the collection and examination of various variables such as gender, age, symptoms, adherence and non-adherence scores. Results were presented in tables and graphs using Microsoft Word and Excel.
RESULTS
Age Distribution Frequency
In our study involving 90 male patients, the age distribution was as follows: 5.55% (n=5) were in the 40-50 years age group, 30% (n=27) in the 51-60 years group, 28.88% (n=26) in the 61-70 years group, 27.77% (n=25) in the 71-80 years group and 7.77% (n=7) in the 81-90 years group (Table 1).
| Sl. No. | Age (year) | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1. | 40-50 | 5 | 5.55 |
| 2. | 51-60 | 27 | 30 |
| 3. | 61-70 | 26 | 28.88 |
| 4. | 71-80 | 25 | 27.77 |
| 5. | 81-90 | 7 | 7.77 |
Frequency of Body Mass Index (BMI)
Of the 90 patients examined, 27.77% (n=25) were classified as having a healthy body weight according to their Body Mass Index (BMI). 40% (n=36) were categorized as overweight, while 32.22% (n=29) were classified as obese (Table 2a).
Within the obese category, 0.1% was categorized as class 1, 96.55% as class 2 and 3.44% as class 3 (Table 2b).
| Sl. No. | BMI | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1. | Healthy weight | 25 | 27.77 |
| 2. | Over weight | 36 | 40 |
| 3. | Obesity | 29 | 32.22 |
| Sl. No. | Obese Patients | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Class 1 | 0 | 0 |
| 2 | Class 2 | 28 | 96.55 |
| 3 | Class 3 | 1 | 3.44 |
Frequency of Social History
Among the patients, 16.66% (n=15) had a smoking habit, while 8.88% (n=8) reported consuming alcohol. Additionally, 36.6% (n=33) of patients reported both smoking and alcohol consumption, while 37.77% (n=34) reported neither habit (Table 2c).
| Sl. No. | Social History | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Smoker | 15 | 16.66 |
| 2 | Alcoholic | 8 | 8.88 |
| 3 | Both | 33 | 36.66 |
| 4 | None | 34 | 37.77 |
Frequency of Occupational Status
Out of the total patients, 64.4% (n=58) were employed, while 35.5% (n=32) were unemployed (Table 2d).
| Sl. No. | Occupation | No. of Patients | Frequency (%) |
|---|---|---|---|
| 1 | Employed | 58 | 64.44 |
| 2 | Unemployed | 32 | 35.55 |
Baseline Assessment of BPH using IPSS
In our research, we assessed the baseline IPSS scores of 90 patients. Of these, 37.77% (n=34) had mild symptoms, 48.88% (n=44) had moderate symptoms and 13.33% (n=12) had severe symptoms (Table 3a; Figure 1).
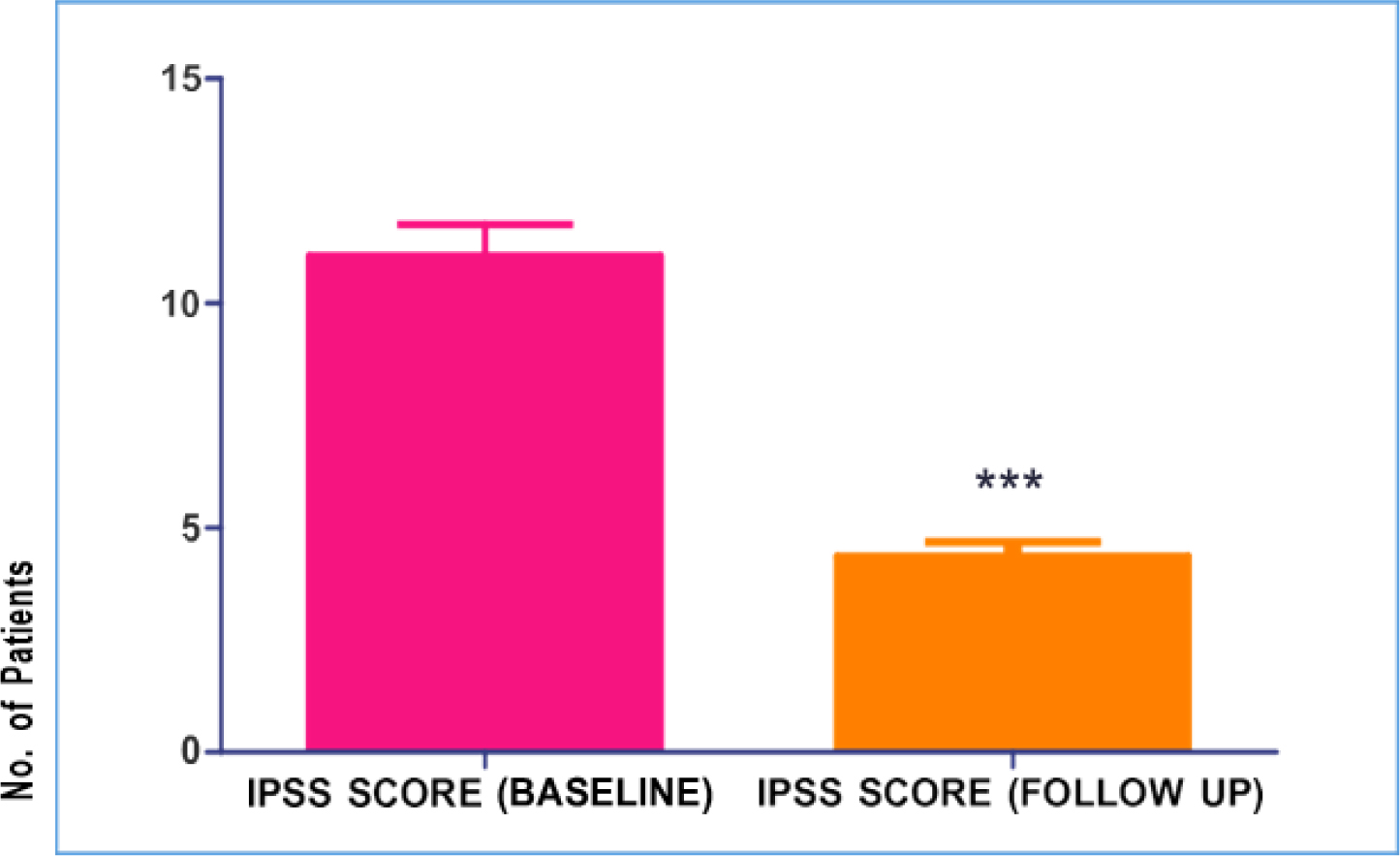
Figure 1:
Mean Difference between IPSS (Baseline) Vs IPSS (Follow-up). Values are expressed as Mean±SEM analysed by paired t-test Graph pad PRISM software. IPSS Score (Follow-up) p<0.0001 as compared with IPSS Score (Baseline). Mean±SEM of IPSS Score (Baseline) is 11.06±0.692, Mean±SEM of IPSS Score (Follow-up) is 4.360±0.318.
| Sl. No. | IPSS (Baseline) | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Mild | 34 | 37.77 |
| 2 | Moderate | 44 | 48.88 |
| 3 | Severe | 12 | 13.33 |
Follow-up Assessment of BPH using IPSS
In our study, we analyzed the follow-up IPSS scores of 90 patients. Among them, 86.66% (n=78) had mild symptoms, 13.3% (n=12) had moderate symptoms and none (0%, n=0) had severe symptoms (Table 3b; Figure 1).
| Sl. No. | IPSS (follow-up) | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Mild | 78 | 86.66 |
| 2 | Moderate | 12 | 13.33 |
| 3 | Severe | 0 | 0% |
Baseline Morisky Medication Adherence Scale
In our study, we evaluated medication adherence at baseline among 90 patients. Of these, 46.66% (n=42) were adherent to their medication regimen, while 53.33% (n=48) were non-adherent (Table 3c).
| Sl. No. | MMAS (baseline) | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Adherent | 42 | 46.66 |
| 2 | Non-adherent | 48 | 53.33 |
Follow-up Morisky Medication Adherence Scale
In our study, among 90 patients, 95.55% (n=86) were found to adhere to their medication, while 4.44% (n=4) were non-adherent (Table 3d).
| Sl. No. | MMAS (follow-up) | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Adherent | 86 | 95.55 |
| 2 | Non-adherent | 4 | 4.44 |
Assessment of Symptom Patterns
Within our study, we observed the prevalence of Lower Urinary Tract Symptoms (LUTS) across eight distinct symptoms. Notably, the highest reported symptoms were nocturia and frequency, noted in 85.5% and 72.2% of cases respectively. Urgency followed closely as the second most prevalent symptom, affecting 62.2% of participants. Intermittency and weak stream were reported less frequently, with incidences of 31% and 26.6% respectively. Straining, dysuria and burning micturition were the least reported symptoms, observed in 12.2%, 15.5% and 8.8% of cases respectively (Table 4).
| Sl. No. | Symptoms | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Frequency | 65 | 72.2 |
| 2 | Urgency | 56 | 62.22 |
| 3 | Weak Stream | 24 | 26.66 |
| 4 | Straining | 11 | 12.22 |
| 5 | Nocturia | 77 | 85.55 |
| 6 | Intermittency | 28 | 31.1 |
| 7 | Dysuria | 8 | 8.88 |
| 8 | Burning Micturition | 14 | 15.55 |
Evaluation of Treatment Patterns
Within our study cohort of 90 patients, 75.55% (n=68) were undergoing monotherapy, while 24.44% (n=22) were undergoing combination therapy (Table 5a).
| Sl. No. | Category | No. of Patients | Percentage (%) |
|---|---|---|---|
| 1 | Monotherapy | 68 | 75.55 |
| 2 | Combination Therapy | 22 | 24.44 |
Distribution of Treatment Patterns
Among the 90 patients in our study, medication prescriptions varied: 26.66% (n=24) received silodosin, 46.66% (n=42) received tamsulosin, 2.22% (n=2) received dutasteride, 3.33% (n=3) received a combination of tamsulosin and dutasteride and 21.11% (n=19) were prescribed a combination of silodosin and dutasteride (Table 5b).
| Sl. No. | Category | Drugs | No. of Patients | Percentage (%) |
|---|---|---|---|---|
| 1 | Monotherapy | Silodosin | 24 | 26.66 |
| Tamsulosin | 42 | 46.66 | ||
| Dutasteride | 2 | 2.22 | ||
| 2 | Combination Therapy | Tamsulosin+Dutasteride | 3 | 3.33 |
| Silodosin+Dutasteride | 19 | 21.11 |
DISCUSSION
Benign Prostate Hyperplasia (BPH) is a prevalent condition among aging men, characterized by the non-cancerous enlargement of the prostate gland, leading to urinary symptoms and potential complications. As men age, hormonal changes, particularly an increase in Dihydrotestosterone (DHT) levels, contribute to prostate growth, making older individuals more susceptible to BPH (Roehrborn, 2010; Miernik and Gratzke, 2020). This demographic trend is of significant concern given the global aging population, underscoring the importance of effective BPH management strategies.
Our study, conducted within the controlled environment of a hospital setting, was designed to address two pivotal aspects of BPH care: medication adherence and symptom control. Medication adherence plays a critical role in managing BPH, as pharmacotherapy, such as alpha-blockers and 5-alpha reductase inhibitors, are commonly prescribed to alleviate symptoms and prevent complications (McVaryet al., 2011; Plochocki and King, 2022). However, non-adherence to medication regimens is a common challenge in chronic disease management, leading to suboptimal treatment outcomes and increased healthcare costs.
Moreover, symptomatic relief is a primary goal in BPH management, as urinary symptoms, including frequency, urgency, nocturia, weak urinary stream and incomplete bladder emptying, significantly impact patients’ quality of life (Oelkeet al., 2013). Addressing these symptoms effectively requires tailored interventions that not only target the physiological aspects of the condition but also consider the psychosocial factors influencing patient well-being.
By implementing a targeted intervention approach, our study aimed to improve patient outcomes and enhance overall quality of life. This intervention likely encompassed multifaceted component, including educational sessions on BPH management, personalized counseling on medication adherence, lifestyle modifications and regular follow-up assessments to monitor symptom progression and treatment response (Ababnehet al., 2019; Cindoloet al., 2015a). Engaging patients in shared decision-making processes and empowering them to take an active role in managing their condition may have also been integral to the intervention’s success (Eisenet al., 2020; McVary, 2007).
The hospital-based nature of our study provided a controlled environment conducive to implementing and evaluating the intervention’s efficacy. Close collaboration between healthcare providers, including urologists, primary care physicians, nurses and pharmacists, likely facilitated the seamless delivery of care and optimization of treatment strategies tailored to individual patient needs. Overall, our study aimed to contribute to the growing body of evidence on effective BPH management strategies, particularly in enhancing medication adherence and symptom control (Johnsonet al., 2020; Kalpan, 2020; Folkvordet al., 2024). By addressing these key aspects of care within a hospital setting, we sought to improve patient outcomes, reduce disease burden and ultimately enhance the quality of life for individuals living with BPH (De Nunzioet al., 2018; Nguyenet al., 2024; Gomelskyet al., 2018).
Our study revealed several key findings regarding the demographic characteristics, clinical presentations and treatment patterns among male BPH patients. The majority of patients fell within the 51-80 years age range, with the highest prevalence observed in the 61-70 years group (Roehrborn, 2010). This aligns with existing literature indicating that BPH primarily affects older men. Moreover, a considerable proportion of patients were overweight or obese, highlighting the potential influence of lifestyle factors on BPH development and progression (Parsonset al., 2011).
Social history factors such as smoking and alcohol consumption were prevalent among the study population. These findings underscore the importance of addressing lifestyle modifications alongside medical interventions in managing BPH (McVaryet al., 2011). Additionally, the high prevalence of employment among patients suggests the need for interventions that accommodate busy work schedules to improve treatment adherence.
Our study assessed BPH symptom severity using the International Prostate Symptom Score (IPSS) both at baseline and follow-up. Interestingly, while moderate symptoms were predominant at baseline, the majority of patients reported mild symptoms at follow-up. This suggests that the intervention implemented in our study may have contributed to symptom improvement over time. Notably, the intervention appeared to have a substantial impact on medication adherence, as evidenced by the significant increase in adherence rates from baseline to follow-up (Saccoet al., 2012; Cindoloet al., 2015b).
The assessment of symptom patterns revealed common symptoms such as nocturia and frequency, which are known to significantly impact patients’ quality of life (Oelkeet al., 2013). The intervention likely played a role in managing these symptoms effectively, contributing to the overall improvement in symptom severity observed during the follow-up period (Nicholet al., 2009).
Furthermore, our study evaluated treatment patterns and found that most patients were undergoing monotherapy, with tamsulosin being the most commonly prescribed medication. However, a notable proportion of patients were on combination therapy, indicating the need for individualized treatment approaches based on symptom severity and patient response.
Overall, our findings suggest that interventions aimed at enhancing medication adherence and symptom management can lead to improved outcomes in BPH patients. Future research should focus on identifying specific components of such interventions that are most effective in promoting adherence and symptom relief. Additionally, exploring the long-term effects of these interventions on disease progression and healthcare utilization would provide further insights into optimizing BPH management strategies.
CONCLUSION
In conclusion, the study conducted at SVIMS Hospital, Tirupati, highlights the significant role of pharmaceutical services in improving medication adherence and subsequently alleviating bothersome symptoms in patients with Benign Prostatic Hyperplasia (BPH). Through pharmaceutical intervention, there was a notable enhancement in adherence, potentially leading to a reduction in symptom severity and an improvement in patients’ overall quality of life. Moreover, the study emphasizes the importance of clinical pharmacists not only in advising patients on medication adherence but also in establishing a meaningful connection between symptom relief and adherence attitudes, thereby fostering a deeper understanding among patients. Ultimately, these findings underscore the pivotal role of pharmaceutical services in the comprehensive management of BPH.
Cite this article:
Yaidikar L, Hemasruthi K, Jasmitha M, Jyothipriya N, Karunakaran K, Kumar NA. Enhancing Medication Adherence and Symptom Management in Benign Prostate Hyperplasia Patients: A Hospital-Based Intervention Study. J Young Pharm. 2025;17(3):724-31.
ACKNOWLEDGEMENT
The authors would like to thank SVIMS-SPMCW for providing necessary facilities.
ABBREVIATIONS
| BPH | Benign Prostate Hyperplasia |
|---|---|
| LUTS | Lower Urinary Tract Symptoms |
| IPSS | International Prostate Symptom Score |
| MMAS-8 | Morisky Medication Adherence Scale (8-item version) |
| DHT | Dihydrotestosterone |
| AUA | American Urological Association |
| BMI | Body Mass Index |
| SPSS | Statistical Package for the Social Sciences |
| SEM | Standard Error of the Mean |
| t-test | Student’s t-test |
| Tamsulosin | A medication used for treating symptoms of BPH |
| Dutasteride | A medication used for treating BPH |
| 5ARI | 5-alpha reductase inhibitors |
| SPSS | Statistical Package for the Social Sciences |
| MMAS | Morisky Medication Adherence Scale. |
References
- Aaron L., Franco O. E., Hayward S. W.. (2016) Review of prostate anatomy and embryology and the etiology of benign prostatic hyperplasia. The Urologic Clinics of North America 43: 279-288 https://doi.org/10.1016/j.ucl.2016.04.012 | Google Scholar
- Ababneh M., Shamieh D., Al Demour S., Rababa’h A.. (2019) Evaluation of the clinical pharmacist role in improving clinical outcomes in patients with lower urinary tract symptoms due to benign prostatic hyperplasia. International Journal of Clinical Pharmacy 41: 1373-1378 https://doi.org/10.1007/s11096-019-00896-2 | Google Scholar
- Al Makahleh B., Sattar A. T., Thorakkattil S., Al Betiri A., Al Hazza H., Nemr H., Jabbour R., Ghamdi F., et al. (2023) Pharmacist-led benign prostatic hyperplasia medication management to an optimal goal in the ambulatory care settings: A longitudinal study. Saudi Journal of Clinical Pharmacy 2: 125 https://doi.org/10.4103/sjcp.sjcp_31_23 | Google Scholar
- Barry M. J., Fowler F. J., O’Leary M. P., Bruskewitz R. C., Holtgrewe H. L., Mebust W. K., Cockett A. T., et al. (1992) The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. The Journal of Urology 148: 1549-57; https://doi.org/10.1016/s0022-5347(17)36966-5 | Google Scholar
- Carrero-López V. M., Cózar-Olmo J. M., Miñana-López B.. (2016) Benign prostatic hyperplasia and lower urinary tract symptoms. A review of current evidence [Hiperplasia prostática benigna y síntomas del tracto urinario inferior. Revisión de las evidencias actuales]. Actas Urologicas Españolas 40: 288-294 https://doi.org/10.1016/j.acuro.2015.12.008 | Google Scholar
- Cindolo L., Pirozzi L., Fanizza C., Romero M., Tubaro A., Autorino R., De Nunzio C., Schips L., et al. (2015a) Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: Population-based cohort study. European Urology 68: 418-425 https://doi.org/10.1016/j.eururo.2014.11.006 | Google Scholar
- Cindolo L., Pirozzi L., Sountoulides P., Fanizza C., Romero M., Castellan P., Antonelli A., Simeone C., Tubaro A., de Nunzio C., Schips L., et al. (2015b) Patient’s adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: Is combination therapy better than monotherapy?. BMC Urology 15: 96 https://doi.org/10.1186/s12894-015-0090-x | Google Scholar
- De Nunzio C., Presicce F., Lombardo R., Trucchi A., Bellangino M., Tubaro A., Moja E., et al. (2018) Patient centred care for the medical treatment of lower urinary tract symptoms in patients with benign prostatic obstruction: A key point to improve patients’ care-A systematic review. BMC Urology 18: 62 https://doi.org/10.1186/s12894-018-0376-x | Google Scholar
- Egan K. B.. (2016) The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: Prevalence and incident rates. The Urologic Clinics of North America 43: 289-297 https://doi.org/10.1016/j.ucl.2016.04.001 | Google Scholar
- Eisen C., Lulic Z., Palacios-Moreno J. M., Adalig B., Hennig M., Cortes V., Gilg F., Kostev K., et al. (2020) Persistence and adherence to dutasteride/tamsulosin fixed-dose versus free-combination alpha blocker/5ARI therapy in patients with benign prostate hyperplasia in Germany. In International Journal of Clinical Pharmacology and Therapeutics 58: 37-49 https://doi.org/10.5414/CP203549 | Google Scholar
- Folkvord F., Würth A. R.-U., van Houten K., Liefveld A. R., Carlson J. I., Bol N., Krahmer E., Beets G., Ollerton R. D., Turk E., Hrubos-Strøm H., Nahoui H., Einvik G., Schirmer H., Moen A., Barrio-Cortes J., Merino-Barbancho B., Arroyo P., Fico G., Lupiáñez-Villanueva F., et al. (2024) A systematic review on experimental studies about patient adherence to treatment. Pharmacology Research and Perspectives 12: Article e1166 https://doi.org/10.1002/prp2.1166 | Google Scholar
- Ghaderi R., Abdollahi Z., Hamidi Madani M., Ghorbani Doshantapeh A., Moghimi B., Jarang M., Rezaei J., Ghaffariyan S., Jafari Arismani R., et al. (2024) Association between serum vitamin D levels and prostate tumor: A systematic review and meta-analysis. Journal of Renal Injury Prevention 13: Article e34296 https://doi.org/10.34172/jrip.2024.34296 | Google Scholar
- Gomelsky A., Kelly E. F., Dalton D. C.. (2018) Combination treatment for male lower urinary tract symptoms with anticholinergic and alpha-blockers. Current Opinion in Urology 28: 277-283 https://doi.org/10.1097/MOU.0000000000000489 | Google Scholar
- Johnson A. T., Jayakumar V., Varghese P. A., Vijayan K., Martin B.. (2020) Impact of educational intervention on medication adherence, quality of life, knowledge attitude and practice among benign prostate hyperplasia patients: A prospective study. International Journal of Basic and Clinical Pharmacology 9: 1807-1815 https://doi.org/10.18203/2319-2003.ijbcp20205115 | Google Scholar
- Kaplan S. A.. (2020) Re: Evaluation of the clinical pharmacist role in improving clinical outcomes in patients with lower urinary tract symptoms due to benign prostatic hyperplasia. The Journal of Urology 204: 1354 https://doi.org/10.1097/JU.0000000000001268 | Google Scholar
- Kaplan S. A.. (2022) Benign prostatic hyperplasia. The Journal of Urology 208: 1323-1325 https://doi.org/10.1097/JU.0000000000002948 | Google Scholar
- Langan R. C.. (2019) Benign prostatic hyperplasia. Primary Care 46: 223-232 https://doi.org/10.1016/j.pop.2019.02.003 | Google Scholar
- Lerner L. B., McVary K. T., Barry M. J., Bixler B. R., Dahm P., Das A. K., Gandhi M. C., Kaplan S. A., Kohler T. S., Martin L., Parsons J. K., Roehrborn C. G., Stoffel J. T., Welliver C., Wilt T. J., et al. (2021) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE part I-Initial work-up and medical management. The Journal of Urology 206: 806-817 https://doi.org/10.1097/JU.0000000000002183 | Google Scholar
- McVary K. T.. (2006) BPH: Epidemiology and comorbidities. The American Journal of Managed Care 12: Array-S128 https://doi.org/10.1097/JU.0000000000002183 | Google Scholar
- McVary K. T.. (2007) A review of combination therapy in patients with benign prostatic hyperplasia. Clinical Therapeutics 29: 387-398 https://doi.org/10.1016/s0149-2918(07)80077-4 | Google Scholar
- McVary K. T., Roehrborn C. G., Avins A. L., Barry M. J., Bruskewitz R. C., Donnell R. F., Foster H. E., Gonzalez C. M., Kaplan S. A., Penson D. F., Ulchaker J. C., Wei J. T., et al. (2011) Update on AUA guideline on the management of benign prostatic hyperplasia. The Journal of Urology 185: 1793-1803 https://doi.org/10.1016/j.juro.2011.01.074 | Google Scholar
- Miernik A., Gratzke C.. (2020) Current treatment for benign prostatic hyperplasia. Deutsches Ärzteblatt International 117: 843-854 https://doi.org/10.3238/arztebl.2020.0843 | Google Scholar
- Mobley D., Feibus A., Baum N.. (2015) Benign prostatic hyperplasia and urinary symptoms: Evaluation and treatment. Postgraduate Medicine 127: 301-307 https://doi.org/10.1080/00325481.2015.1018799 | Google Scholar
- Morisky D. E., Ang A., Krousel‐Wood M., Ward H. J.. (2008) Predictive validity of a medication adherence measure in an outpatient setting. Journal of Clinical Hypertension 10: 348-354 https://doi.org/10.1111/j.1751-7176.2008.07572.x | Google Scholar
- Nguyen T., Truong M. T. X., Lam D. N., Nguyen H. T. T., Huynh A. M., Duong V. K., Vo T. P. M., Nguyen T. H., Cao T. T. M., Pham S. T., Tran B. L. T., Van Nguyen L., et al. (2024) Effectiveness of clinical pharmacist intervention on medication adherence in patients with chronic obstructive pulmonary disease-A randomized controlled study. Patient Education and Counseling 118: Article 108037 https://doi.org/10.1016/j.pec.2023.108037 | Google Scholar
- Nichol M. B., Knight T. K., Wu J., Barron R., Penson D. F.. (2009) Evaluating use patterns of and adherence to medications for benign prostatic hyperplasia. The Journal of Urology 181: 2214-21; https://doi.org/10.1016/j.juro.2009.01.033 | Google Scholar
- Oelke M., Bachmann A., Descazeaud A., Emberton M., Gravas S., Michel M. C., N’Dow J., Nordling J., de la Rosette J. J., et al. (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. European Urology 64: 118-140 https://doi.org/10.1016/j.eururo.2013.03.004 | Google Scholar
- Parsons J. K., Bergstrom J., Silberstein J., Barrett-Connor E.. (2008) Prevalence and characteristics of lower urinary tract symptoms in men aged ≥80 years. Urology 72: 318-321 https://doi.org/10.1016/j.urology.2008.03.057 | Google Scholar
- Parsons J. K., Messer K., White M., Barrett-Connor E., Bauer D. C., Marshall L. M., et al. (2011) & Osteoporotic Fractures in Men (MrOS) Research Group and the Urologic Diseases in America Project. European Urology. JK 60: 1173-1180 https://doi.org/10.1016/j.eururo.2011.07.040 | Google Scholar
- Plochocki A., King B.. (2022) Medical treatment of benign prostatic hyperplasia. The Urologic Clinics of North America 49: 231-238 https://doi.org/10.1016/j.ucl.2021.12.003 | Google Scholar
- Roehrborn C. G.. (2011) Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). The Medical Clinics of North America 95: 87-100 https://doi.org/10.1016/j.mcna.2010.08.013 | Google Scholar
- Sacco E., Bientinesi R., Marangi F., Totaro A., D’Addessi A., Racioppi M., Pinto F., Vittori M., Bassi P., et al. (2012) Patient-reported outcomes in men with lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) treated with intraprostatic onabotulinumtoxinA: 3-month results of a prospective single-armed cohort study. BJU International Array: E837-E844 https://doi.org/10.1111/j.1464-410X.2012.11288.x | Google Scholar
- Yeaw J., Benner J. S., Walt J. G., Sian S., Smith D. B.. (2009) Comparing adherence and persistence across 6 chronic medication classes. Journal of Managed Care Pharmacy: JMCP 15: 728-740 https://doi.org/10.18553/jmcp.2009.15.9.728 | Google Scholar