ABSTRACT
Background
Stroke, a leading cause of death and disability, is primarily classified into ischemic and hemorrhagic types. Red Cell Distribution Width, measures the variability in red blood cell size, is an emerging biomarker linked to stroke severity. The primary aim of this study was to evaluate the utility of Red Cell Distribution Width in predicting stroke severity and to assess potential drug-drug interactions that could lead to adverse drug reactions in acute ischemic stroke patients.
Materials and Methods
This study was conducted over a six-month period and included 120 patients diagnosed with cerebral infarction. Red Cell Distribution Width and other parameters were measured and correlated with stroke severity using the National Institutes of Health Stroke Scale and Glasgow Coma Scale scores. The patients were monitored throughout their stay. Pearson correlation analysis was employed for data evaluation.
Results
Among 120 patients, 75% were male and 25% were female, with majority of patients aged between 55 and 85 years. The results indicated significantly higher values in patients with severe strokes (p value <0.001). A positive correlation was observed between Red Cell Distribution Width and the standard stroke score (r=0.11), while a weak negative correlation was found with Glasgow Coma Scale score (r=-0.04). Hemoglobin also exhibited a weak negative correlation with stroke severity. Drug-drug interactions were identified in 39% of patients, and adverse drug reactions included nasal bleeding and hematuria.
Conclusion
Red Cell Distribution Width is a promising and accessible biomarker for assessing the severity of acute ischemic stroke and the associated mortality risk.
INTRODUCTION
Stroke is one of the leading causes of death, with rates over 41.1 per 100,000 in 2021 (Feigin et al., 2021). According to Disability-Adjusted Life Years (DALYs), stroke is the second leading cause of death and the third leading cause of death with disability worldwide, the first being ischemic heart disease (Maet al., 2021). It is divided into ischemic and hemorrhagic stroke. Diagnosis is primarily achieved via neuroimaging and neurological assessment tools such as the National Institutes of Health Stroke Scale (NIHSS) and the Canadian Neurological Scale (CNS). Timely diagnosis and intervention are crucial in stroke cases, as they significantly influence patient outcomes by reducing mortality and long-term disability (Gulatiet al., 2021).
In recent years, Red Cell Distribution Width (RDW)–a parameter quantifying the variability in Red Blood Cell (RBC) sizes–has garnered attention as a prognostic indicator in Acute Ischemic Stroke (AIS) (Demiret al., 2015). It is a standard parameter included in Complete Blood Count (CBC) tests. Elevated RDW levels are associated with increased inflammation and oxidative stress (Zhanget al., 2021; Ghazizadehet al., 2020), which are critical factors in many diseases, including cardiovascular conditions and strokes. Numerous studies have demonstrated a strong association between high RDW levels and adverse outcomes in cardiovascular diseases and stroke (Daneseet al., 2015). For instance, higher RDW levels have been linked to greater stroke severity and poorer prognosis (Eyiol and Ertekin, 2024). While neuroimaging techniques are the foundation for AIS diagnosis, biochemical examination of cell damage may serve as a supplementary technique for preliminary assessment. A biomarker to identify and screen for AIS patients could be beneficial, especially for those who may benefit from thrombolytic therapy prior to hospitalization (Kouet al., 2022).
The integration of RDW as a predictive tool not only holds potential in individual patient care but also serves as a vital element in broader public health initiatives (Zhanget al., 2022). By providing an affordable and accessible means of assessing stroke severity, RDW contributes to a more equitable distribution of diagnostic resources, addressing disparities in healthcare access. Furthermore, ischemic stroke patients often contend with comorbidities and polypharmacy, which elevate the risk of Drug-Drug Interactions (DDIs). The increased susceptibility to these interactions can significantly alter the intended therapeutic effects, potentially leading to adverse outcomes. Timely identification of such interactions is essential for preventing adverse effects and may necessitate adjustments to the treatment plan.
This study aims to elucidate the potential of RDW as a predictive biomarker for AIS severity, correlating with established scoring scales (NIHSS and Glasgow Coma Scale), investigate the relationship between anemia and acute ischemic stroke, and evaluate the occurrence and implications of DDIs and Adverse Drug Reactions (ADRs) in this patient population. By exploring these objectives, the study seeks to enhance understanding of RDW in stroke prognosis and inform clinical practices to improve patient outcomes.
MATERIALS AND METHODS
This prospective observational study was conducted over a period of six months, from November 2023 to April 2024. Participants included in the study were patients diagnosed with AIS, confirmed through clinical evaluation and imaging studies. Inclusion criteria required that patients be aged 18 years or older and provide informed consent. Exclusion criteria included patients with haemorrhagic stroke, other significant comorbid conditions that could influence RDW levels (e.g., chronic inflammatory diseases, malignancies), or incomplete medical records. Before enrollment, all patients or their legal representatives were informed about the study’s objectives, procedures, potential risks, and benefits. Consent was documented in writing, adhering to ethical standards and ensuring compliance with institutional and regulatory guidelines.
The severity of AIS in patients was assessed using the National Institutes of Health Stroke Scale (NIHSS) and the Glasgow Coma Scale (GCS) scores. These scales provided standardized measures of neurological impairment and stroke severity. Blood samples were collected to measure RDW, complete blood count, lipid profile, C-reactive Protein (CRP), and cardiac function tests. Throughout the hospital stay, patients were closely monitored for potential Drug-Drug Interactions (DDIs) and Adverse Drug Reactions (ADRs). This monitoring was essential for understanding the impact of medication regimens on patient outcomes and ensuring safe and effective treatment. The relationships between RDW, haemoglobin levels, and stroke severity were analysed using Pearson correlation coefficients. This statistical method allowed for the assessment of the strength and direction of the linear relationships between these variables, providing insights into the potential role of RDW as a biomarker for AIS severity.
RESULTS
Demographics
Out of 120 patients included in the study, 90 (75.00%) were male and 30 (25.00%) were female. The age group with the highest incidence of Acute Ischemic Stroke (AIS) was 61-70 years, accounting for 37 patients (30.83%). Hypertension was the most prevalent comorbidity, observed in 80 patients (66.67%), followed by diabetes mellitus in 27 patients (22.50%). Demographic details of the study population are summarized in Table 1.
| Characteristic | n (%) (n=120) |
|---|---|
| Gender | |
| Male | 90 (75.00) |
| Female | 30 (25.00) |
| Age (years) | |
| 21-30 | 2 (1.67) |
| 31-40 | 7 (5.83) |
| 41-50 | 22 (18.33) |
| 51-60 | 35 (29.16) |
| 61-70 | 37 (30.83) |
| 71-80 | 16 (13.33) |
| 81-90 | 1 (0.83) |
| Major Risk Factors | |
| Hypertension | 34 (28.33) |
| Diabetes | 27 (22.50) |
| Smoking | 14 (12.00) |
| Ischemic heart disease | 9 (7.50) |
| Overweight | 4 (3.30) |
| Chest pain | 3 (2.50) |
| Hypothyroidism | 2 (1.66) |
| Hyperthyroidism | 1 (0.83) |
| Valve replacement | 1 (0.83) |
| Asthma | 1 (0.83) |
Red Cell Distribution Width and Stroke Severity
Correlation with National Institutes of Health Stroke Scores
RDW was found to follow the upward trend along with stroke severity, as examined using NIHSS. The mean RDW progressively increased with 14.56±1.59 in minor strokes, 14.97±1.53 in moderate strokes, 15.41±1.74 in moderate to severe strokes, and 17.32±3.02 in severe strokes. This steady rise was statistically significant (p<0.001), with a Pearson correlation coefficient of 0.384.
Correlation with Glasgow Coma Scale Scores
Similarly, RDW values also showed a statistically significant relationship with Glasgow Coma Scale (GCS) scores. Patients with minor, moderate, and severe strokes had mean RDW levels in the rising levels of 15.33±2.16, 15.95±1.70, and 16.74±3.02, respectively. The overall correlation between GCS and RDW was negative (r=-0.309, p<0.001), with the strongest negative correlation observed in severe stroke patients (r=-0.75) (Table 2).
| Severity Index | Correlation coefficient | p-value |
|---|---|---|
| National Institutes of Health Stroke Scale | ||
| Mild | 0.4401 | <0.001 |
| Moderate | 0.0714 | <0.001 |
| Moderate to Severe | 0.0139 | <0.001 |
| Severe | 0.0197 | <0.001 |
| Glasgow Coma Scale | ||
| Mild | -0.022 | 0.017 |
| Moderate | -0.274 | 0.086 |
| Severe | -0.756 | <0.001 |
Haemoglobin Levels and Stroke Severity
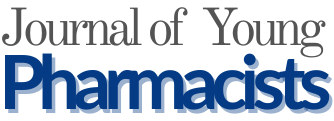
In contrast, haemoglobin levels were inversely associated with stroke severity. The mean RDW followed a declining trend with 14.31±1.35 (median=13.95) in patients with minor stroke, 12.64±2.07 (median=13) in moderate stroke patients, 12.44±2.70 (median=12.7) in patients with moderate to severe stroke, and 11.22±2.13 (median=11.3) in severe stroke patients. These differences were statistically significant (p<0.001), with an overall correlation coefficient of 0.356 (Figure 1).
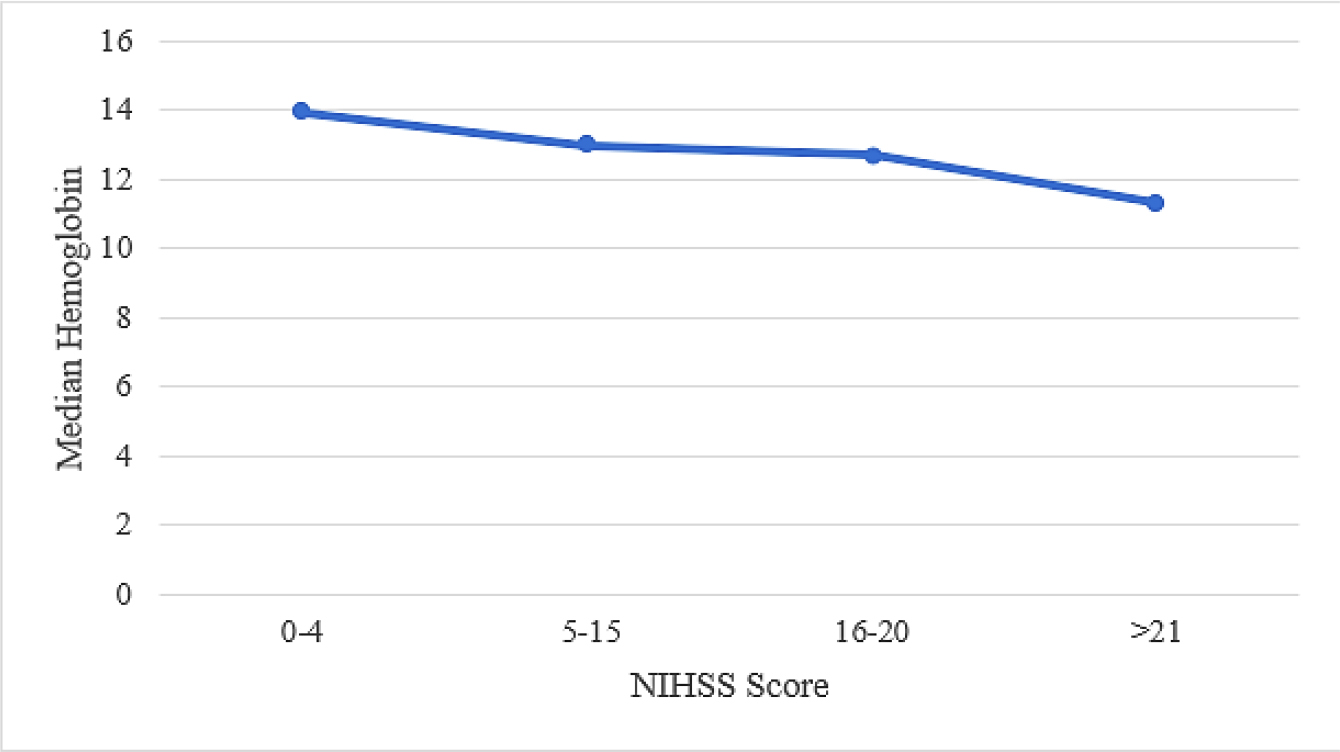
Figure 1:
Relationship between NIHSS score and median hemoglobin levels in AIS patients. The graph shows a decreasing trend in hemoglobin levels with increasing stroke severity based on NIHSS categories. Reproduced at 91.54 mm column width.
Comparison of Red Cell Distribution Width with Mortality in Patients
A majority of the patients (96%) were discharged after a variable hospital stay of 2-8 days while 4% of the patients died. Figure 2 shows that RDW values were correspondingly lower in surviving patients (median=13.8) than in patients who expired (median=15.5) indicating an emerging mortality predictor (p-value=0.048).
Figure 2:
Comparison of median RDW values based on patient status (expired vs discharged). The chart indicates higher RDW levels in patients who expired, suggesting a potential association with poorer outcomes. Reproduced at 94.72 mm column width.
Commonly Prescribed Drugs in Patients
In total, 95 medications were prescribed to the patients with AIS. Pantoprazole was prescribed in 99 patients out of 120 and was the most common drug (82.5%), followed by Ondansetron (75%), Clopidogrel (68.4%), and Aspirin (62.5%). Other commonly used medications included lipid-lowering agents (67.5%), antibiotics (53.4%), antiepileptics, hypoglycemics, antihypertensives, and lactulose.
Drug Interactions
A total of 52 drug interactions were identified in the patients with AIS, with majority being present in males. The most common drug classes (Figure 3) prescribed to AIS patients were anti-platelets, anti-hypertensives, and lipid-lowering agents, followed by antidiabetics, antipsychotics, and PPIs. The incidence rate of drug-drug interaction was 39.13%. Management of these interactions included drug withdrawal in 25.8% of cases, biochemical monitoring in 12.48%, and close symptomatic observation in 14.14% of subjects. In uncommon cases (0.83%), suspected drugs were switched.
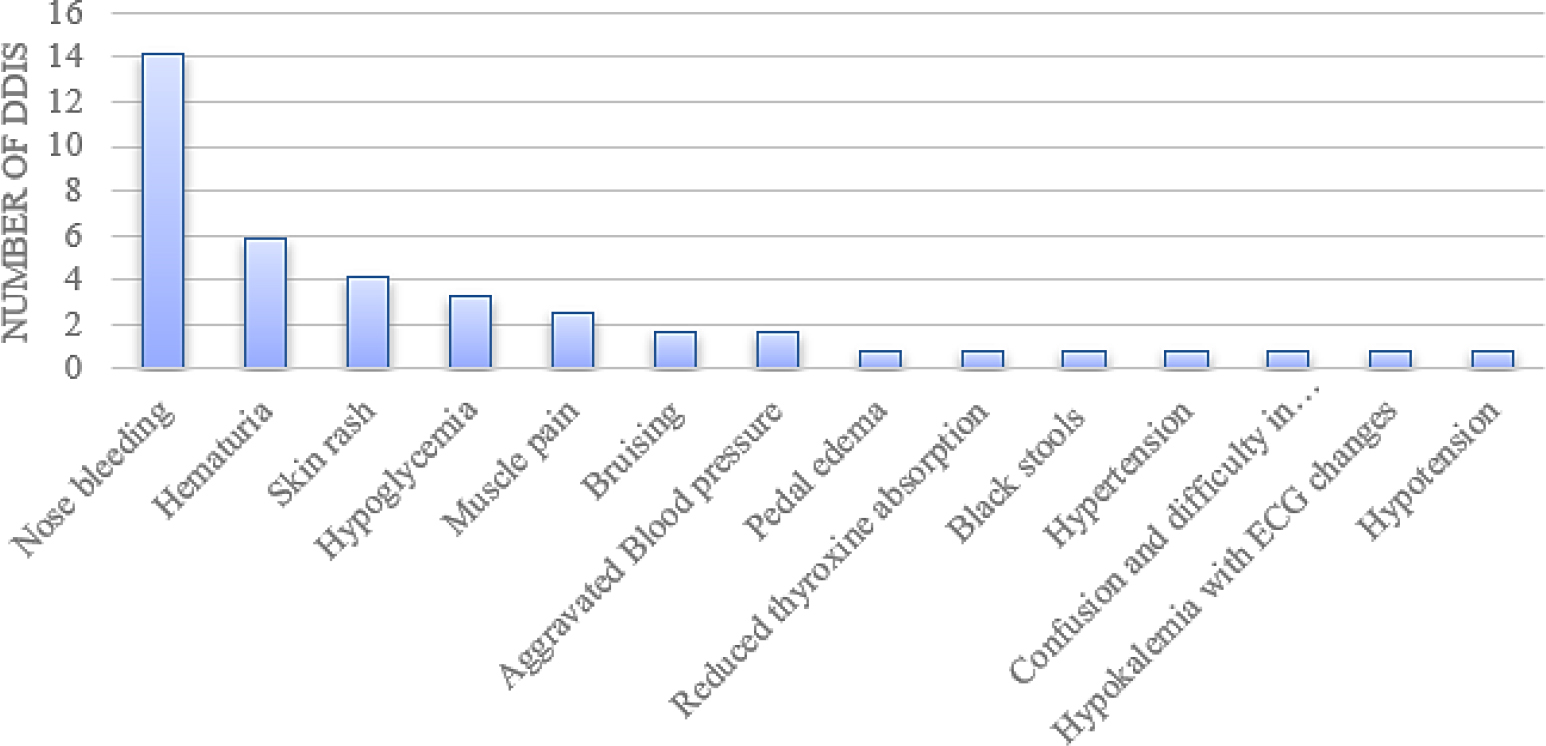
Figure 3:
Frequency of drug-drug interactions observed among patients with acute ischemic stroke. The figure highlights the most common interacting drug classes used during inpatient care. Reproduced 86.78 mm column width.
Adverse Drug Reactions in Patients
Table 3 provides a summary of Adverse Drug Reactions (ADRs) occurring in AIS patients. Hematuria and anemia were the most common adverse events observed. Most ADRs involved antiplatelets and antifibrinolytics. Patients aged 51-90 years mostly experienced ADRs. Some notable cases included heparin-induced hematuria, atenolol-induced bradycardia, and tranexamic acid- and aspirin-clopidogrel-induced anemia. In all these cases, the suspected medications were discontinued, and follow-up investigations confirmed symptom resolution.
| ADRs found | Number of cases | Percentage (n=120) (%) |
|---|---|---|
| Tranexamic acid-induced severe anemia | 2 | 2 |
| Heparin-induced Hematuria | 1 | 0.83 |
| Atenolol-induced Bradycardia | 1 | 0.83 |
| Clopidogrel-Aspirin induced anemia | 1 | 0.83 |
DISCUSSION
Acute Ischemic Stroke (AIS) is a prime cause of morbidity and mortality worldwide, demanding rapid diagnosis and prognostic evaluation for early management. While neuroimaging is required for evaluation, there is a need for a quick and easy test for predicting the severity of stroke, which can improve recovery rates and lessen the overall burden on healthcare systems (Xuet al., 2022). RDW, being a standard component of complete blood count tests, offers a cost-effective and readily available measure for early diagnosis and treatment planning in AIS patients.
RDW was previously investigated as an indicator of inflammation in cases of acute myocardial infarction (Wisselet al., 2014) and peripheral vascular disease (Shenet al., 2022). It is related to acute ischemic stroke through mechanisms involving inflammation and oxidative stress (Joosseet al., 2023), which lead to atherosclerosis, subsequently elevating the likelihood of ischemic stroke (Konget al., 2022). This process can also impact the structure of Red Blood Cells (RBCs) by modifying membrane proteins (Pretorius, 2018), leading to an extended lifespan of RBCs and premature release of larger RBCs into the peripheral circulation, thus increasing RDW (Chunget al., 2022).
Our study results found that elevated RDW levels are positively correlated with stroke severity, as measured by NIHSS and GCS scores. Our observations align with Feng et al., (2017), who conducted a meta-analysis and determined that there is a probable link between elevated RDW and conditions such as ischemic cerebrovascular disease, carotid artery atherosclerosis, and cerebral embolism (Fenget al., 2017). Furthermore, Sarhan et al., (2019) reported that RDW values higher than 14.6 significantly increased stroke risk by multiple folds, with an odds ratio of 4.38 (p<0.001), indicating that higher RDW levels are associated with poorer clinical outcomes and reinforcing its potential as a reliable biomarker (Sarhan et al., 2019b).
In relation to our research, it was analyzed that the median RDW was higher in deceased patients (15.5) compared to those discharged alive (13.8), with a statistically significant correlation (p=0.048). Previous studies also reported higher RDW levels in expired AIS patients; for instance, Ani and colleagues (2009) discovered that individuals with RDW values exceeding 13.9% were twice as likely to face mortality compared to the reference group (Ani and Ovbiagele, 2008). This suggests a potential link between RDW and AIS mortality.
The study also examined the relationship between hemoglobin levels and stroke severity, revealing a statistically significant negative correlation with NIHSS scores. This indicates that as stroke severity increased, hemoglobin levels decreased–a finding consistent with prior research by Tanné et al., where 19% of severe AIS patients had anemia (Tanneet al., 2010). Although the correlations were weak, hemoglobin levels still provide valuable information about the overall health status of stroke patients. Monitoring hemoglobin can help assess the patient’s capacity to transport oxygen, which is critical in stroke recovery management (Kaiafa et al., 2016).
Our study also highlighted the prevalence of Drug-Drug Interactions (DDIs) and Adverse Drug Reactions (ADRs). Antiplatelets and cholesterol-lowering medications were the most frequently prescribed drugs. However, prophylactic medications such as antibiotics, proton pump inhibitors, and anti-emetics were also commonly used. The prevalence and clinical implications of DDIs and ADRs were mainly associated with anticoagulants and antiplatelets. An incidence rate of 39.13% for DDIs underscores the importance of vigilant therapeutic monitoring.
ADRs observed included events such as hematuria and anemia, primarily linked to heparin, clopidogrel, aspirin, and tranexamic acid. Our findings support previous research indicating that the geriatric population is particularly susceptible to ADRs due to age-related physiological changes and comorbidities, emphasizing the importance of post-marketing surveillance and prompt withdrawal of suspected drugs upon ADR detection.
These observations collectively validate the study hypothesis that hemoglobin and RDW levels are closely associated with stroke severity, and that judicious drug management is essential in AIS patients. Incorporating RDW into standard diagnostic algorithms may facilitate early risk stratification and guide clinical decision-making, especially in resource-limited settings. Additionally, reviewing medication charts and performing interaction checks can reduce the burden of preventable drug-related problems.
Nevertheless, this study has some limitations. The small sample size and relatively short duration may affect the generalizability of the results. The observed associations might have been influenced by potential confounding factors not fully accounted for, such as pre-existing comorbidities and varying treatment approaches. Larger, multicentric studies are necessary to validate these findings.
Future research should aim to validate RDW as a reliable biomarker for stroke severity across diverse populations and clinical settings. Investigating the optimal timing for RDW measurement in relation to stroke onset could also enhance its clinical utility. Longitudinal studies assessing RDW’s role in stroke risk stratification, prognosis prediction, and post-stroke recovery would provide deeper insights into its potential applications.
CONCLUSION
A comprehensive analysis of RDW, hemoglobin, commonly prescribed drugs, drug interactions, and adverse drug reactions in AIS patients sheds light on the intricate landscape of stroke management. These findings underscore the critical role of monitoring biomarkers, managing drug regimens, and promptly addressing ADRs and DDIs to optimize patient outcomes and ensure the safety and efficacy of treatment strategies in the context of acute ischemic stroke. By delving deeper into the observed trends and addressing the limitations of small sample size and limited study duration, future research can pave the way for improved stroke prevention, early intervention, and ultimately, better patient outcomes.
Cite this article:
Gladwin E, Patel M, Shah R, Mistry D, Mishra A, Shah A, et al. A Cross-Sectional Observational Study to Assess Red Cell Distribution Width as a Novel Biomarker for the Prediction of Severity of Acute Ischemic Stroke. J Young Pharm. 2025;17(3):691-6.
ABBREVIATIONS
| DALY | Disability-Adjusted Life Year |
|---|---|
| NIHSS | National Institutes of Health Stroke Scale |
| CNS | Canadian Neurological Scale |
| RDW | Red Cell Distribution Width |
| CBC | Complete Blood Count |
| AIS | Acute Ischemic Stroke |
| DDI | Drug-Drug Interaction |
| GCS | Glasgow Coma Scale |
| ADR | Adverse Drug Reaction |
| CRP | C-Reactive Protein |
| PPI | Proton Pump Inhibitor. |
References
- Ani C., Ovbiagele B.. (2009) Elevated red blood cell distribution width predicts mortality in persons with known stroke. Journal of the Neurological Sciences 277: 103-108 https://doi.org/10.1016/j.jns.2008.10.024 | Google Scholar
- Chung Y., Desiraju S., Namachivayam K., Guzman P., He L., MohanKumar K., et al. (2022) Hematological changes in neonatal mice with phlebotomy-induced anemia. Pediatric Research 92: 1575-1579 https://doi.org/10.1038/s41390-022-02023-w | Google Scholar
- Danese E., Lippi G., Montagnana M.. (2015) Red blood cell distribution width and cardiovascular diseases. Journal of Thoracic Disease 7: E402-E411 https://doi.org/10.3978/j.issn.2072-1439.2015.10.04 | Google Scholar
- Demir R., Saritemur M., Atis O., Ozel L., Kocaturk İ. EMet, Emet M., Ulvi H., et al. (2015) Can we distinguish stroke and stroke mimics via red cell distribution width in young patients?. Archives of Medical Science 11: 958-963 https://doi.org/10.5114/aoms.2014.40995 | Google Scholar
- Eyiol A., Ertekin B.. (2024) The relationship between hemoglobin-to-red cell distribution width (RDW) ratio (HRR) and mortality in stroke patients. European Review for Medical and Pharmacological Sciences 28: 1504-1512 https://doi.org/10.26355/eurrev_202402_35480 | Google Scholar
- Feng G.-H., Li H.-P., Li Q.-L., Fu Y., Huang R.-B.. (2017) Red blood cell distribution width and ischaemic stroke. Stroke and Vascular Neurology 2: 172-175 https://doi.org/10.1136/svn-2017-000071 | Google Scholar
- GBD 2019 Stroke Collaborators. (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet. Neurology 20: 795-820 https://doi.org/10.1016/S1474-4422(21)00252-0 | Google Scholar
- Ghazizadeh H., Mirinezhad M. R., Seyedi S. M. R., Sadabadi F., Ahmadnezhad M., Jaberi N., Pasdar A., Ferns G. A., Esmaily H., Ghayour-Mobarhan M., et al. (2020) Prognostic factors associating with pro-oxidant-antioxidant balance; neutrophils to lymphocytes ratio, vitamin D, heat shock protein 27, and red cell distribution width. Archives of Medical Research 51: 261-267 https://doi.org/10.1016/j.arcmed.2020.02.006 | Google Scholar
- Gulati A., Agrawal N., Vibha D., Misra U. K., Paul B., Jain D., Pandian J., Borgohain R., et al. (2021) Safety and efficacy of sovateltide (IRL-1620) in a multicenter randomized controlled clinical trial in patients with acute cerebral ischemic stroke. CNS Drugs 35: 85-104 https://doi.org/10.1007/s40263-020-00783-9 | Google Scholar
- Joosse H.-J., van Oirschot B. A., Kooijmans S. A. A., Hoefer I. E., van Wijk R. A. H., Huisman A., van Solinge W. W., Haitjema S., et al. (2023)
In vitro and in silico evidence for oxidative stress as drivers for RDW. Scientific Reports 13: 9223 https://doi.org/10.1038/s41598-023-36514-5 | Google Scholar - Kaiafa G., Savopoulos C., Kanellos I., Mylonas K. S., Tsikalakis G., Tegos T., Kakaletsis N., Hatzitolios A., et al. (2017) Anemia and stroke: Where do we stand?. Acta Neurologica Scandinavica 135: 596-602 https://doi.org/10.1111/ane.12657 | Google Scholar
- Kong P., Cui Z.-Y., Huang X.-F., Zhang D.-D., Guo R.-J., Han M., et al. (2022) Inflammation and atherosclerosis: Signaling pathways and therapeutic intervention. Signal Transduction and Targeted Therapy 7: 131 https://doi.org/10.1038/s41392-022-00955-7 | Google Scholar
- Kou J., Gu X., Kang L.. (2022) Correlation analysis of computed tomography features and pathological types of multifocal ground-glass nodular lung adenocarcinoma. Computational and Mathematical Methods in Medicine 2022: Article 7267036 https://doi.org/10.1155/2022/7267036 | Google Scholar
- Ma Q., Li R., Wang L., Yin P., Wang Y., Yan C., Ren Y., Qian Z., Vaughn M. G., McMillin S. E., Hay S., Naghavi M., Cai M., Wang C., Zhang Z., Zhou M., Lin H., Yang Y., et al. (2021) Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: An analysis for the Global Burden of Disease Study 2019. The Lancet. Public Health 6: e897-e906 https://doi.org/10.1016/S2468-2667(21)00228-0 | Google Scholar
- Moun Sarhan A. A., El-Sharkawy K. A., Elkhatib T. H., Mohamed Hassan A. A.. (2019) Red blood cell distribution width as a predictor of clinical outcome in acute ischemic stroke patients. International Journal of Clinical and Experimental Neurology 7: 12-16 https://doi.org/10.1016/S2468-2667(21)00228-0 | Google Scholar
- Pretorius E.. (2018) Erythrocyte deformability and eryptosis during inflammation, and impaired blood rheology. Clinical Hemorheology and Microcirculation 69: 545-550 https://doi.org/10.3233/CH-189205 | Google Scholar
- Shen T., Yang X., Zhang Z.. (2022) Positive relationship of RDW with NT-proBNP and cTnI in acute myocardial infarction patients. Clinical Laboratory 68 https://doi.org/10.7754/Clin.Lab.2021.210808 | Google Scholar
- Tanne D., Molshatzki N., Merzeliak O., Tsabari R., Toashi M., Schwammenthal Y., et al. (2010) Anemia status, hemoglobin concentration and outcome after acute stroke: A cohort study. BMC Neurology 10: 1-7 https://doi.org/10.7754/Clin.Lab.2021.210808 | Google Scholar
- Wissel J., Verrier M., Simpson D. M., Charles D., Guinto P., Papapetropoulos S., Sunnerhagen K. S., et al. (2015) Post‐stroke spasticity: Predictors of early development and considerations for therapeutic intervention. PM and R 7: 60-67 https://doi.org/10.1016/j.pmrj.2014.08.946 | Google Scholar
- Xu Q., Ou X., Li J.. (2022) The risk of falls among the aging population: A systematic review and meta-analysis. Frontiers in Public Health 10: Article 902599 https://doi.org/10.3389/fpubh.2022.902599 | Google Scholar
- Zhang L., Huang T., Xu F., Li S., Zheng S., Lyu J., Yin H., et al. (2022) Prediction of prognosis in elderly patients with sepsis based on machine learning (random survival forest). BMC Emergency Medicine 22: 26 https://doi.org/10.1186/s12873-022-00582-z | Google Scholar
- Zhang Y., Xing Z., Zhou K., Jiang S.. (2021) The predictive role of systemic inflammation response index (SIRI) in the prognosis of stroke patients. Clinical Interventions in Aging 16: 1997-2007 https://doi.org/10.2147/CIA.S339221 | Google Scholar