ABSTRACT
Background
Hypertension increases the risk of cerebrovascular illness and cognitive decline by directly affecting the cerebral artery vasomotor function causing premature death. As the retina and the brain have similar embryological origins, any microvascular alterations in the retina can detect subtle changes in the cerebral vasculature, which can be used to suspect the diagnosis of cerebral dysfunctions. The purpose of our study is to determine an association between Hypertensive Retinopathy (HTRP) and stroke.
Materials and Methods
This is a prospective observational study, 240 hypertensive patients were selected based on the inclusion criteria involving all age groups, Patients’ information was gathered using patient data collecting forms and the following were obtained: Demographic details, medical history, diagnosis and laboratory data was obtained. The data was sorted according to JNC-8 criteria and Keith-Wagner Classification for HTRP and entered into Microsoft excel and analyzed using SPSS software 26 version and the association was determined using Pearson chi-square and Pearson correlation.
Results
Out of 240 hypertensive patients 196 had stroke and 84 had HTRP. The association between HTRP and stroke was assessed in 40 individuals with both stroke and HTRP, A Pearson chi-square showed that there is a significant association between the two variables at 0.05 level [χ2 (4, N=40)=10.952a, p=.027)]. Conclusion: From our study we conclude that there is a statistically significant (p=<0.05) association between HTRP and stroke. Hence it is necessary to promote diagnosis of HTRP as an indicator for stroke.
INTRODUCTION
A stroke is a medical emergency that occurs when there is a sudden interruption of continuous blood flow to the brain. This interruption can be due to a blocked or restricted blood artery in the brain, or it can occur due to a blood vessel rupture and leaking blood into the brain.1
Retinal blood vessels normally experience reversible vasoconstriction in response to acute blood pressure increase and optic disc oedema may result from hypertensive crisis. Exudative vascular alterations result from endothelial injury and necrosis in more severe or chronic hypertension. Hypertension-related retinal vascular damage is known as Hypertensive Retinopathy (HTRP). The distinctive characteristics of retinal blood vessels that set them apart from other blood vessels are: Lacking sympathetic nerve supply, the self-regulation of blood flow, presence of blood-retinal barrier. As a result, the constricting arteries directly experience an increase in blood pressure. However, an increase in blood pressure that exceeds this compensatory tone damages the muscular and endothelial layers.2
The following is brought on by persistent, poorly managed hypertension: Constant vascular narrowing, unusual arteriovenous crossing (arteriovenous nicking), arteriosclerosis with mild to moderate alterations in the vascular wall (copper wiring) to more severe hyperplasia and thickening of the vascular wall (silver wiring). One of the main risk factors for the emergence of a branch retinal vein blockage is arteriovenous nicking.3 The optic nerve and retina protrude from the growing brain during embryonic development. The eyes are the only organs in the human body that display the central nervous system and blood vasculature. Several major neurodegenerative illnesses that affect the brain and spinal cord show retinal symptoms, implying that the eye is the brain’s “window”.4 Due to the same embryological origins, architectural features, and physiological characteristics of retinal and cerebral small arteries, ocular signs of stroke are to be predicted.5,6 BBB or BRB dysfunction is thought to have a key role in the development of cerebral and retinal microangiopathy, respectively.7,8
It’s significant to note that alterations in retinal vascularization are evident early in the disease process, whereas BBB collapse typically goes unnoticed until there has been significant vasogenic oedema and brain damage.9
The transparent media of the eye allows non-invasive visualization of the retina in vivo, thus changes in the vasculature of the eye can be early indicators of neurological diseases such as multiple sclerosis or stroke. For example, if pressure in the brain increases due to hypertension or a brain tumor, it can cause swelling of the optic nerve, which can be seen through an eye examination.10,11 Therefore, an inexpensive, five-minute eye scan can accurately assess the amount of brain damage in people with stroke and offer clues about how quickly the disease is progressing.12 The purpose of our study is to determine an association between HTRP and stroke.
MATERIALS AND METHODS
This study included in-patients who were admitted to the Vivekananda General Hospital, Deshpande Nagar Hubballi. This is a Prospective observational study (Study flow chart: Figure 1). This study was conducted for a period of 1 year. The sample was calculated by using the formula based on the pilot study which was estimated to be 240.
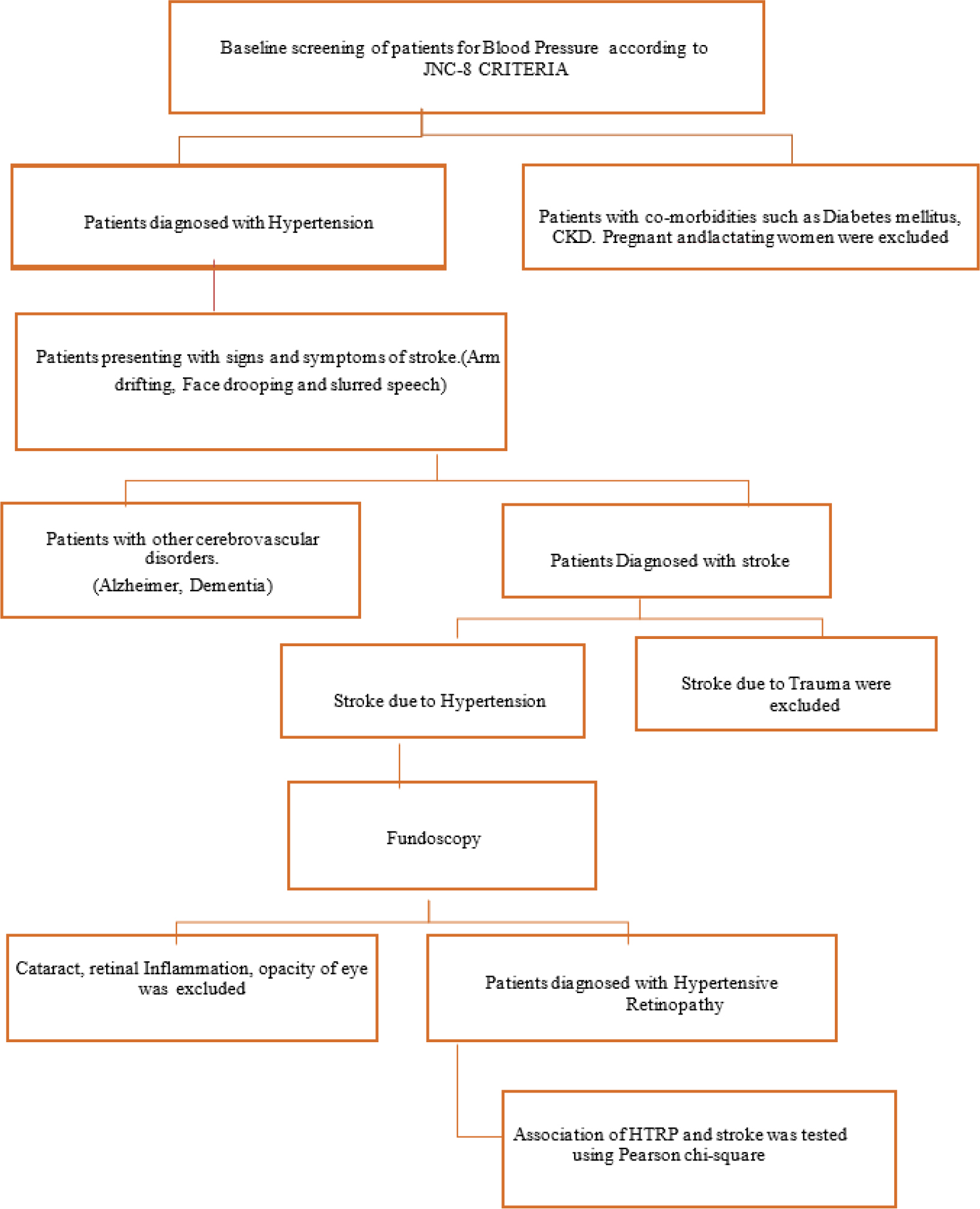
Figure 1:
Study Flow Chart.
Inclusion Criteria
Patients above 18 years of age, Patients with known case of Hypertension, Patients diagnosed with hypertensive stroke, Patients of known case of hypertensive stroke, Patients with diagnosed with HTRP, Patients of both genders.
Exclusion Criteria
Patients having pre-existing retinal vasculopathy changes other than hypertension, Patients having pre-existing media opacity such as corneal opacity and cataract that precludes dilated fundus examination, Patients having diabetes, Patients with active ocular inflammation or infection, Pregnant and lactating women.
Data Analysis
The patient data were collected and sorted according to JNC-8 criteria and Keith Wagner Classification for HTRP. The data was entered in Microsoft Excel with the IP no, The entered data were analyzed using SPSS version 26, All the data were uploaded in SPSS and analyzed by various parametric and non-parametric test like Pearson chi- square and Pearson correlation, Normality distribution was analyzed. Data was not normally distributed, hence non-parametric analysis was used.
Ethical Considerations
Ethical clearance for this study was obtained from the Institutional Ethical Committee KLE College of Pharmacy, Hubballi to carry out this research project. IEC Number: KLECOPH/ IEC/2022-23/03.
RESULTS
This study included a total of 240 patients among which 179 were male (75%) and 61 were females (25%) Age groups 60-69 and 70-79 years were in majority accounting for 48.7% of the total population (Figure 2), with minimum patients in 20-29 and 90-99 years of age group i.e., 3.7%. 24(10%) and 62(26%) of the total population were included in smoking and drinking alcohol respectively and 216(90%) and 178(74%) were non- smokers and non-alcoholics respectively (Table 1).
| Sl. No. | Demographics and Social History | Male | Female |
|---|---|---|---|
| 1. | Individuals | 179 (75%) | 61 (25%) |
| 2. | Smoking | 24 (10%) | 0 |
| 3. | Non-Smokers | 0 | 216 (90%) |
| 4. | Alcoholic | 62 (26%) | 0 |
| 5. | Non-Alcoholic | 0 | 178 (74%) |
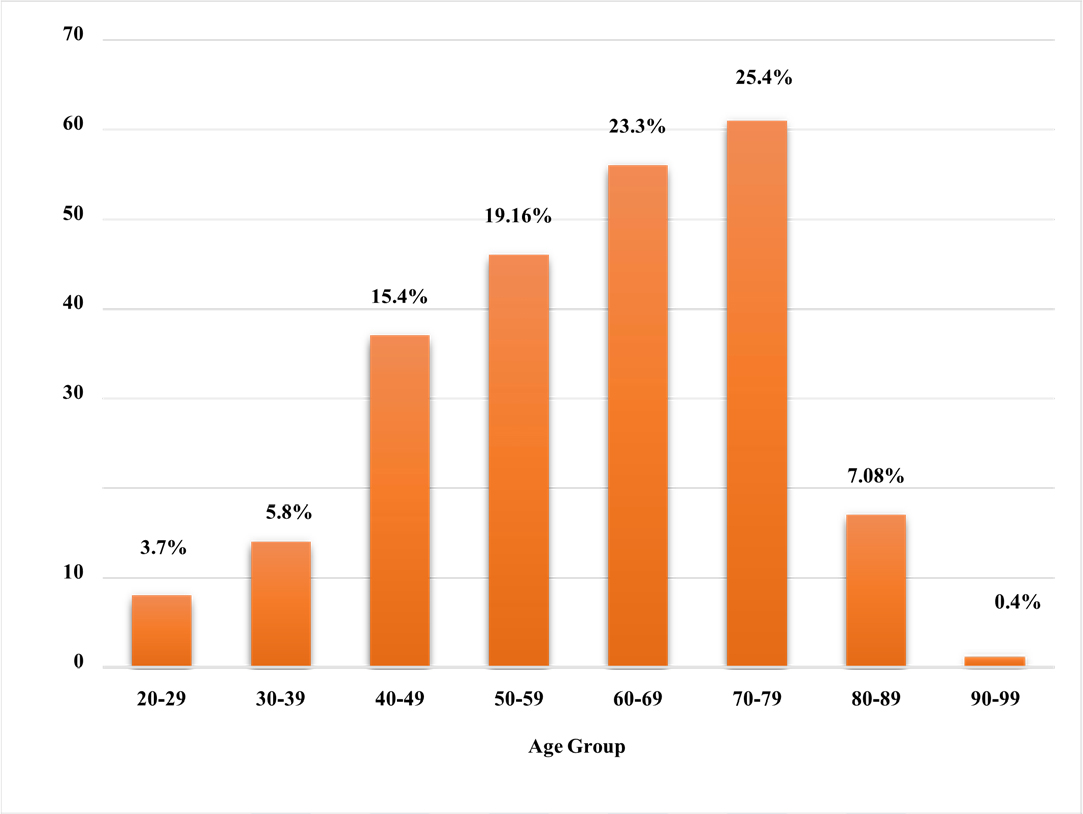
Figure 2:
Distribution of Study Population (N=240) based on age.
We classified hypertensive patients based on JNC-8 criteria i.e., Normal blood pressure (SBP less than 120 mmHg and DBP less than 80 mmHg), Prehypertension (SBP 120-139 mmHg or DBP 80-89 mmHg) Stage 1 hypertension (SBP 140-159 mmHg or DBP 90-99 mmHg) and Stage 2 hypertension (SBP 160 mmHg or higher or DBP 100 mmHg or higher. According to our findings, the majority of the patients i.e,133 (55.4%) had stage-2 SBP and 113(47.08%) had DBP (Table 2). 196 hypertensive patients (out of 240) suffered a stroke. There were 133 (68%) new hospitalizations for stroke (first stroke), 35 (18%) recurrent stroke cases and 28 (14%) with a history of stroke. According to our findings, 158 males (80.61%) had a higher risk of stroke than females 19.39% (38). When compared to hemorrhagic stroke 79 (40.3%) and TIA 10(5.1%), the prevalence of ischemic stroke was high 107 incidences (54.6%). Males aged 50-59 (hemorrhagic stroke) and 70-79 (ischemic stroke) and females aged 60-69 (1-HS and 3-IS) had a higher chance of getting a stroke (Tables 3 and 4).
| Sl. No. | Stages of SBP and DBP | No. of Patients with SBP | No. of Patients with DBP |
|---|---|---|---|
| 1 | Normal | 4 (1.66%) | 17 (7.08%) |
| 2 | Prehypertension | 19 (7.9%) | 45 (18.7%) |
| 3 | Stage 1 | 84 (35%) | 65 (27.08%) |
| 4 | Stage 2 | 133 (55.4%) | 113 (47.08%) |
| Total | 240 | 240 |
On determining the associations of risk factors with that of stroke, we observed that out of 196 stroke patients, the prevalence of smoking and alcohol was 21 (10.72%) and 57 (29.08%) respectively (Table 3). An association of risk factors with stroke was analyzed, the results showed a significant association at 0.05 level [χ2 (2, N=196)=9.587a, p=.008)] with smoking and an insignificant association was observed with stroke and alcohol (p=0.385) (Table 5).
| Association of variables with Stroke | |||
|---|---|---|---|
| Variables | Value | Df | Asymptotic Significance (2-sided) |
| Gender and Stroke Types Pearson Chi-Square | 2.594 | 2 | 0.273 |
| Smoking and Stroke Pearson Chi-Square | 9.587 | 2 | 0.008* |
| Alcohol and Stroke Pearson Chi-Square | 1.908 | 2 | 0.385 |
| SBP and Stroke Pearson correlation (N=196) | 0.172 | 1 | 0.016* |
| DBP and Stroke Pearson correlation (N=196) | 0.157 | 1 | 0.028* |
| Stoke and HTRP Pearson Chi-Square | 10.952 | 4 | 0.027* |
| Age Group | Female | Male | Total | ||||
|---|---|---|---|---|---|---|---|
| Hemorrhage | Ischemia | TIA | Hemorrhage | Ischemia | TIA | ||
| 20-29 | 1 | 0 | 0 | 4 | 2 | 0 | 7 |
| 30-39 | 0 | 1 | 0 | 2 | 6 | 0 | 9 |
| 40-49 | 1 | 4 | 0 | 13 | 11 | 1 | 30 |
| 50-59 | 2 | 1 | 1 | 19 | 15 | 1 | 39 |
| 60-69 | 2 | 3 | 0 | 19 | 22 | 4 | 50 |
| 70-79 | 5 | 10 | 1 | 8 | 22 | 2 | 48 |
| 80-89 | 0 | 6 | 0 | 3 | 3 | 0 | 12 |
| 90-99 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| TOTAL | 11 | 25 | 2 | 68 | 82 | 8 | 196 |
In our study, the mean and standard deviation of SBP and DBP were 162.8+27.17 and 92.4+12.27, respectively. To examine the association between Systolic blood pressure, Diastolic blood pressure and stroke, a Pearson correlation coefficient was calculated. The two variables had a positive association, with r (196)=[.172*], p=[.016] and r (196)=[.157**], p=[.028] respectively (Table 5).Newly diagnosed hypertensive individuals are more prone to get ischemic and hemorrhagic strokes and as the duration of hypertension extends the likelihood of having an ischemic stroke increase (Figure 3).
| Sl. No. | Stroke | No. of Patients | Total |
|---|---|---|---|
| Distribution of Gender | |||
| 1. | Male | 158 (80.61%) | 196 |
| 2. | Female | 38 (19.36%) | |
| Stroke occurrence | |||
| 3. | New Hospitalizations | 133 (68%) | 196 |
| 4. | Recurrent cases | 35 (18%) | |
| 5. | Old cases | 28 (14%) | |
| Types of Strokes | |||
| 6. | Hemorrhage | 79 (40.3%) | 196 |
| 7. | Ischemic | 107 (54.6%) | |
| 8. | TIA | 10 (5.1%) | |
| Distribution of smokers and non-smokers in stroke patients | |||
| Smoker | Yes | No | 196 |
| 9. | Hemorrhage | 8 | 71 |
| 10. | Ischemic | 9 | 98 |
| 11. | TIA | 4 | 6 |
| Distribution of Alcoholics based on Types of Strokes | |||
| Alcoholic | Yes | No | 196 |
| 12. | Hemorrhage | 26 | 53 |
| 13. | Ischemic | 27 | 80 |
| 14. | TIA | 4 | 6 |
| Occurrence of Seizure in Stroke patients | |||
| Seizure Occurrence | Yes | No | 196 |
| 15. | Hemorrhage | 15 | 64 |
| 16. | Ischemic | 21 | 86 |
| 17. | TIA | 2 | 8 |
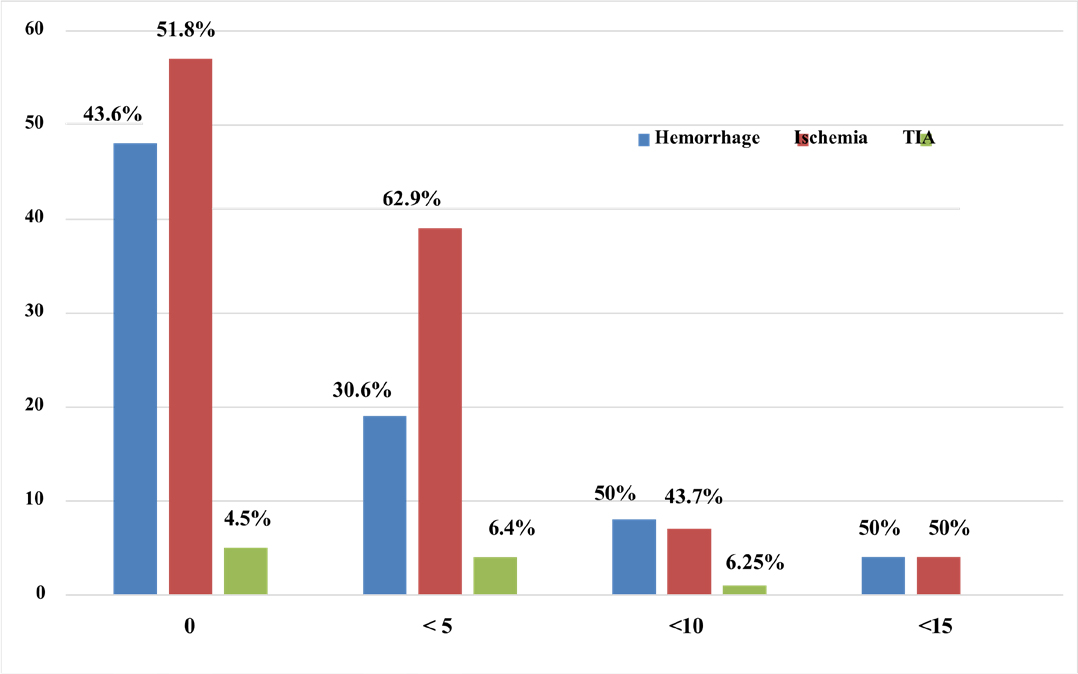
Figure 3:
Distribution of Duration of HTN and Type of Stroke.
The major complication of stroke is seizure. In our study the prevalence of seizure occurrence was 19.39% and more frequent in patients with ischemic stroke (55.23%) (Table 3).
84 out of 240 hypertensive patients had HTRP. Age groups between 60 and 79, with a mean age of 62.07 had a greater risk of developing HTRP. It was observed that males had higher chances of getting grade-1 HTRP and females were more prone to get grade-2 HTRP (Table 6).
| Sl. No. | HTRP | No. of Patients | Total |
|---|---|---|---|
| Distribution of Gender | |||
| 1. | Male | 51 | 84 |
| 2. | Female | 33 | |
| Grades of HTRP | |||
| 3. | Grade-1 | 52 | 84 |
| 4. | Grade-2 | 21 | |
| 5. | Grade-3 | 11 | |
| Distribution of smokers and non-smokers in HTRP patients | |||
| Smoker | Yes | No | 84 |
| 6. | Grade-1 | 6 | 46 |
| 7. | Grade-2 | 0 | 21 |
| 8. | Grade-3 | 1 | 10 |
| Distribution of Alcoholics | |||
| Alcoholic | Yes | No | 84 |
| 9. | Grade-1 | 12 | 40 |
| 10. | Grade-2 | 3 | 18 |
| 11. | Grade-3 | 1 | 10 |
In this study, we observed that grade 1 (61%) HTRP had higher prevalence among ischemic stroke patients when compared to other retinopathy grades that age groups between 70 and 79 years were more likely to have grade 1 HTRP, and that age groups between 50 and59 years were more likely to have grade 2 HTRP (Figure 4). Males are more likely to get HTRP than females. The Relation between age, alcohol, SBP and DBP with HTRP was found to be significant at p=<0.05. A Pearson correlation coefficient was computed to assess the relationship between HTRP and stroke we observed a positive correlation between the two variables, (p=<0.05) (Table 7).
| Variables | Value | Asymptotic Significance (2-sided) |
|---|---|---|
| Age and HTRP Spearman Correlation (N=84) | 0.222 | 0.042* |
| Smoking and HTRP Pearson Chi-Square (N=84, df=3) | 3.976 | 0.264 |
| Alcohol and HTRP Spearman Correlation (N=84) | 0.202 | 0.065* |
| SBP and HTRP Pearson Chi-Square (N=84, df=48) | 128.065 | <.001* |
| DBP and HTRP Pearson Chi-Square (N=84, df=24) | 104.007 | <.001* |
| HTRP and Stroke Pearson’s R (N=40, df=4) | 0.323 | 0.042* |
| Stoke and HTRP Pearson Chi-Square (N=40) | 10.952 | 0.027* |
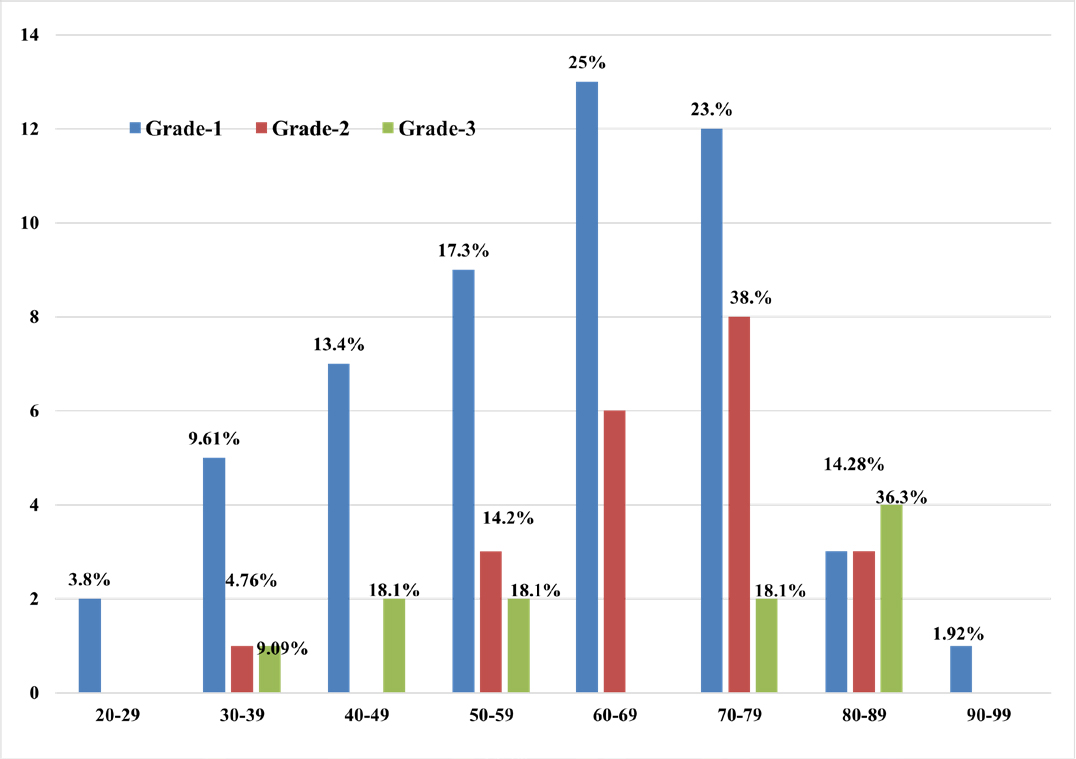
Figure 4:
Distribution of Age group with Grade of HTRP.
DISCUSSION
A retrospective epidemiological study conducted by Sylvan Lavy et al. shows that there was no sex predominance in the hypertensive stroke cases at different age groups,13 but according to our findings, males 80.61% (158) had a higher risk of stroke than females 19.39% (38). Males aged 50-59 (hemorrhagic stroke) and 70-79 (ischemic stroke) and females aged 60-69 (1-HSand 3-IS) had a higher chance of getting a stroke. Sylvan Lavy et al. concluded that hypertension plays an important role in the development of cerebral ischemia and hemorrhage equally,13 our study showed a higher prevalence of ischemic stroke 54.6% (107 incidences) when compared to hemorrhagic stroke 40.3% (79) and TIA 5.1% (10).
The results from SYSTUP-India study conducted by Rishi Sethi et al. showed that 50 years of uncontrolled hypertension can have 4% increased risk of stroke.14 From our study we observed that individuals with new onset hypertension diagnosed with stage-2 HTN (SBP 160 mmHg or higher or DBP 100 mmHg or higher) had a higher risk of stroke especially ischemic stroke. On applying Pearson’s Chi-square to test the association between gender, smoking and alcohol with stroke, our results showed that there is a statistically significant association of smoking with stroke at 0.05 level [χ2 (2, N=196)=9.587a, p=.008)], Whereas gender and alcohol were not statistically significant with stroke. Similarly, the study conducted by Rishi Sethi et al., showed that smoking had the strongest impact on 10-year risk on stroke. Age and SBP are correlated with CV and cerebrovascular disease risk, and it is known that age and HTN are key risk factors for stroke.14
84 out of 240 hypertensive patients had HTRP. Age groups between 60 and 79, with a mean age of 62.07, had a greater risk of developing HTRP. It was observed that males had higher chances of getting grade 1 HTRP and females were more prone to get grade-2 HTRP. A study conducted by Erden et al. showed that the severity and duration of hypertension were directly proportional to the incidence of HTRP and Retinopathy is correlated with increased age and severity of hypertension.15 In our study, we observed that grade-1 (61%) HTRP had higher prevalence among ischemic stroke patients when compared to other retinopathy grades that age groups between 70 and 79 years were more likely to have grade 1 HTRP, and that age groups between 50 and 59 years were more likely to have grade 2 HTRP. Males are more likely to get HTRP than females.
A study conducted by Yi-Ting Ong et al., concluded that HTRP was linked to a higher risk of cerebral infarction in hypertensive that were taking medication and had excellent blood pressure control.16 In our study on computing Pearson correlation coefficient to assess the relationship between HTRP and stroke we observed a positive correlation between the two variables, (p=<0.05). Similarly, a study conducted by Xuling Chen et al. showed a substantial positive correlation between HTRP and the risk of first stroke and first ischemic stroke.17
The limited sample size and time duration are both limitations of this study. One of the study’s shortcomings is that we lack sufficient data of Retinal images and MRI to analyse the degree of association between the two retinal images and brain scan which will undoubtedly be the focus of future research.
CONCLUSION
A sudden and consistent elevation in blood pressure is a major risk factor for target end organ damage, which requires immediate treatment interventions, if not might be fatal. Despite overwhelming evidence that hypertension is the greatest risk factor for stroke and that lowering blood pressure is the most effective strategy of avoiding stroke, predicting who will have one remains difficult. Deciphering novel risk factors or symptoms that may give more information is thus still vital. The effect of hypertension can be easily observed on smaller capillaries. Therefore, the impact of hypertension on eye is very evident, leading to microvascular changes in retina (HTRP). The retinal and cerebral arteries have a common embryological origin with anatomical and structural similarities; hence some significant changes in the retinal microvasculature might detect the fine changes in the cerebral arteries.
In persons with hypertension who do not have diabetes, HTRP is associated with an increased long-term risk of stroke regardless of other vascular risk factors. Even though their blood pressure appears to be under control, those with HTRP are more likely to have a cerebral infarction. The findings of our study shows that simple fundoscopic examination of the retina subsides the risk of stroke by predicting its chances of occurrence, furthermore our study would help the physicians to decide the exact treatment interventions that would reduce the chance of death due tom stroke in hypertensive patients.
Cite this article
Hiremath JS, Swamy AHV, Sridhar T, Varghese LE, Hasharudeen A, Saxena A. Clinical Implications of Retinopathy in Hypertensive Patients: Analyzing the Potential Connection to Stroke Risk. J Young Pharm. 2024;16(1):58-65.
ACKNOWLEDGEMENT
We would like to express sincere thanks to the Management and Principal, KLE College of Pharmacy, Hubballi, Karnataka for providing necessary facilities to carry out research. We owe our hearty thanks to Dr. Sanatkumar B. Nyamagoud, Dr. Abhishek B J, Dr. Santosh B Patil and Dr. Girish Hampannavar faculties of KLE College of Pharmacy for their timely help and support during the course. We would like to take this opportunity to express our sincere thanks to the biostatistician Dr. G.N. Bhadri, for providing us timely guidance for assisting us with statistical data, despite his busy schedule.
ABBREVIATIONS
| BBB | Blood Brain Barrier |
|---|---|
| BRB | Blood Retinal Barrier |
| CV | Cardiovascular |
| DBP | Diastolic Blood Pressure |
| HS | Hemorrhagic Stroke |
| HTN | Hypertension |
| HTRP | Hypertensive Retinopathy |
| IP | In patient |
| IS | Ischemic Stroke |
| JNC-8 criteria | Joint National Committee 8 criteria |
| MRI | Magnetic Resonance Imaging |
| SBP | Systolic Blood Pressure |
| SPSS | Statistical Package for Social Sciences |
| TIA | Transient Ischemic Stroke |
| WHO | World Health Organization |
References
- National Institute of Neurological Disorders and Stroke. [cited Dec 3 2023]. Available fromhttps://www.ninds.nih.gov/search?search_api_fulltext=Neurological+Disorders+and+Stroke%2C2023+Apr+5
- Modi P, Arsiwalla T. Hypertensive retinopathy. StatPearls [Internet]. 2023:2023 [Google Scholar]
- Mehta S. MSD manual professional edition. [cited Dec 3 2023]. Available fromhttps://www.msdmanuals.com/professional/ eye-disorders/retinal-disorders/hypertensive-retinopathy
Hypertensive retinopathy [internet]. - London A, Benhar I, Schwartz M. The retina as a window to the brain-from eye research to CNS disorders. Nat Rev Neurol. 2013;9(1):44-53. [PubMed] | [CrossRef] | [Google Scholar]
- Baker ML, Hand PJ, Wang JJ, Wong TY. Retinal signs and stroke: revisiting the link between the eye and brain. Stroke. 2008;39(4):1371-9. [PubMed] | [CrossRef] | [Google Scholar]
- Patton N, Aslam T, MacGillivray T, Pattie A, Deary IJ, Dhillon B, et al. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: a rationale based on homology between cerebral and retinal micro-vasculatures. J Anat. 2005;206(4):319-48. [PubMed] | [CrossRef] | [Google Scholar]
- Kaur C, Foulds WS, Ling EA. Blood-retinal barrier in hypoxic ischaemic conditions: basic concepts, clinical features and management. Prog Retin Eye Res. 2008;27(6):622-47. [PubMed] | [CrossRef] | [Google Scholar]
- Wardlaw JM, Sandercock PAG, Dennis MS, Starr J. Is breakdown of the blood-brain barrier responsible for lacunar stroke, leukoaraiosis, and dementia?. Stroke. 2003;34(3):806-12. [PubMed] | [CrossRef] | [Google Scholar]
- Cheung N, Mosley T, Islam A, Kawasaki R, Sharrett AR, Klein R, et al. Retinal microvascular abnormalities and subclinical magnetic resonance imaging brain infarct: a prospective study. Brain. 2010;133(7):1987-93. [PubMed] | [CrossRef] | [Google Scholar]
- Gottlob I. The Conversation. 2015 [cited Dec 3 2023]. Available fromhttp://theconversation.com/the-eye-is-our-window-to-the-brain-and-theres-a-lot-we-can-tell-from -it-38746
The eye is our window to the brain-and there’s a lot we can tell from it. - Yap TE, Balendra SI, Almonte MT, Cordeiro MF. Retinal correlates of neurological disorders. Ther Adv Chronic Dis. 2019 10:204062231988220: 2040622319882205 [PubMed] | [CrossRef] | [Google Scholar]
- Hopkinsmedicine.org. [cited Dec 3 2023]. Available fromhttps://www.hopkinsmedicine.org/news/media/releases/using_the_eye_as_a_window_into_the_brain
Using the eye as A ‘window into the brain’; 10/17/2012 [internet]. - Lavy S, Melamed E, Cahane E, Carmon A. Hypertension and diabetes as risk factors in stroke patients. Stroke. 1973;4(5):751-9. [PubMed] | [CrossRef] | [Google Scholar]
- Sethi R, Hiremath JS, Ganesh V, Banerjee S, Shah M, Mehta A, et al. Correlation between stroke risk and systolic blood pressure in patients over 50 years with uncontrolled hypertension: results from the SYSTUP-India study. Cardiovasc Ther. 2021;2021:6622651 [PubMed] | [CrossRef] | [Google Scholar]
- Erden S, Bicakci E. Hypertensive retinopathy: incidence, risk factors, and comorbidities. Clin Exp Hypertens. 2012;34(6):397-401. [PubMed] | [CrossRef] | [Google Scholar]
- Ong YT, Wong TY, Klein R, Klein BEK, Mitchell P, Sharrett AR, et al. Hypertensive retinopathy and risk of stroke. Hypertension. 2013;62(4):706-11. [PubMed] | [CrossRef] | [Google Scholar]
- Chen X, Liu L, Liu M, Huang X, Meng Y, She H, et al. Hypertensive retinopathy and the risk of stroke among hypertensive adults in China. Invest Ophthalmol Vis Sci. 2021;62(9):28 [PubMed] | [CrossRef] | [Google Scholar]
