ABSTRACT
Background
India is among the highest burden of Tuberculosis (TB) cases across the world. Delaying the diagnosis and treatment adherence towards anti TB drugs were common causes observed among the TB patients. There is a need to identify the gaps and provide the awareness about the TB infection, which will help to achieve a ‘TB free India’ by 2025. Therefore, we aim to assess and evaluate the Knowledge, Attitude and Perception (KAP) among TB patients regarding the management of TB.
Materials and Methods
A Randomized controlled study was conducted among TB patients. A Self-prepared and validated KAP questionnaire was developed using World Health Organization (WHO) recommendations for TB KAP studies and interviewed the patients at the baseline. In test group by using patient information leaflets and counselling were given under the clinical pharmacist whereas in control group usual care was given by other health care team. Then two follow ups were done after every three months by using same set of questionnaires in both groups.
Results
A total of 250 participants were enrolled, among 220 were recruited in which majority of them belongs to 26-35 age group in both test 63 (57.27%) and control 66 (60%). In health seeking behaviour, most of them usually go to private clinic compared to government clinic or hospital. In response to TB knowledge and awareness, attitude with stigma and perception at baseline found to be low but at the end of sixth month the parameters were improved among both test and control group. The test group had shown better improved KAP than the control group.
Conclusion
Majority of the participants had inadequate levels of KAP at baseline but got improved in post follow ups among both test and control groups. Test group had shown more improvement compared to control group. Thus, indicating the importance of clinical pharmacist intervention in improving the KAP among TB patients.
INTRODUCTION
Tuberculosis (TB) had come to epidemic extent in many countries including India.1 India has more new cases of TB each year than any other country and has the highest burden of TB, contributing one-fifth to the global burden.2 Among different types, pulmonary TB is one of the leading causes of death in adults followed by MDR TB and HIV/AIDs with TB as it leads every 3 min two people die in our country with TB.3 To combat tuberculosis, in 1962 India’s National Tuberculosis Control Program was launched, later renamed to Revised National Tuberculosis Control Programme (RNTCP) and then National Tuberculosis Elimination Programme (NTEP).4 The aim of this program is to reduce TB mortality and morbidity as well as TB transmission until TB is no longer a major concern for public health.5
The NTEP program uses DOTS (Directly Observed Treatment, Short course) to achieve this goal. To successfully complete the program, it is important that patients have basic and correct knowledge about the disease.6 Since 1970, Knowledge, Attitude and Perception (KAP) research has become the main intervention strategy to fight Tuberculosis (TB) worldwide.7 Several studies have shown that KAP levels in individuals are associated with effective disease management, response to medical treatment, and improvement in their own health.8–11 Lower levels of KAP were considered one of the key factors for poor health, ineffective use of health care services, low screening rates, and inadequate preventive behaviour.12–14 Even in many Indian states have shown evidences in this regard.
Clinical pharmacist’s plays a critical role in clinical settings to improve patient compliance and outcomes. Since many years, pharmacists are involved in patient care and raising awareness about maintenance of good healthcare systems.15 They also have responsibility to involve in national strategy plan in elimination of TB from India by 2025. The common causes that were observed among the TB patients were the diagnosis delay and drug adherence towards anti TB drugs.16 There is a need to identify the gaps, reasons and provide the awareness about the TB infection, which will help to achieve of a ‘TB free India’ by 2025.17 Clinical pharmacist through pharmaceutical care services can educate the TB patients on the basic awareness of KAP might improve in achieving the treatment outcomes.18 Therefore, we aim to study the Knowledge, Attitude and Perception (KAP) among the TB patients in different follow up times in the region of Belagavi of Karnataka state in India.
MATERIALS AND METHODS
Study design and settings
A single-blind randomized controlled study was carried out in a tertiary-care hospital TB center and four Primary Health Care (PHC) centers in the district of Belagavi, Karnataka state in India. The study was carried out between September 2021 to March 2023 on TB patients who were visiting the TB center in tertiary care hospital and followed up back in PHCs. The randomization was performed by two parallel arms divided in a ratio of 1:1 ratio by a simple envelope technique as usual care group (Control) and the pharmaceutical care intervention group (Test). The envelopes were opened in front of pharmacist and study participant were assigned. The test group participants were given pharmaceutical care intervention under a clinical pharmacist in a separate room at TB center in the hospital and control group with usual care under other health care professionals. The clinical pharmacist was the primary person of contact if any problem arises during the study.
Designing and development of questionnaire
A self-framed and validated KAP questionnaire was developed by using World Health Organization (WHO) recommendations for TB KAP studies19 and were interviewed for both test and controls from baseline to follow ups. The questionnaire consisted of yes or no or don’t know type questions and others was developed using 5-point Likert scale. The questionnaire was divided into five sections covering demographic information, health-seeking behaviour, TB knowledge and awareness, TB attitude and stigma and perception on TB. In prior to conduct the main study a pilot study was conducted as the questionnaire got validated from the faculty members of KLE college of pharmacy and reliability was found to be good (Cronbach’s alpha i.e., α >0.83).
Development and validation of Patient Information Leaflets (PILs)
In accordance to WHO and NTEP guidelines, patient information leaflets (PILs) for educating and counselling were prepared in English, Kannada and Marathi languages. A team of respiratory medicine physicians (n=4), pharmacists (n=3), and lay person (n=1) reviewed the leaflets. The readability of the patient information leaflet was assessed using the Flesch Reading Ease (FRE) formula. The FRE scale value ranges from 0 to 100. If the value was less than 60, the leaflet will be difficult to read. The average FRE score is 78, indicating that it was easy to read and understand. The layout and design of the PILs was evaluated using with mean Baker Able Leaflet Design (BALD) score. The values were calculated depending on line length, line spacing, font type and size, indentation, colours, pictures, paper texture etc. The mean BALD score was found to be 25, confirming that the patients were able to read and understand the PILs. The PILs consists of regarding TB and its complications, signs and symptoms, risk factors, ATT drug information, life style changes and modifications.
Study participants
Participants above 18 years old, new diagnosed pulmonary TB and taking self-administered TB treatment both Antitubercular Treatment (ATT) and Fixed Dose Combination therapy (FDC) from private practitioners were included. Participants with extrapulmonary TB, having more than one comorbidity, and not willing to participate were excluded from the study. Participants were explained about the study through subject information sheets and Informed Consent Forms (ICF) was obtained after enrolling into the study.
Data collection
The Participants were interviewed with data collection form which includes demographic details such as age, gender, marital status, religion, area, education level, working experience etc. The participants who were enrolled at the baseline were follow-up for two regular intervals, one at third and final sixth month of TB treatment.
Statistical Analysis
The statistical analysis was carried out by using Microsoft Excel spread sheet and later entered into SPSS V23.0 (IBM, USA). Descriptive analysis was utilized and expressed in frequency, percentage, Mean±SD, and by using independent t test. Tabulations and Bar graphs were used to display the data. The level of significance was kept to be less than 0.05.
Ethical considerations
From the Institutional Ethical Clearance (IEC) for human subjects committee at KLE academy of higher education and research, Belagavi, Karnataka, India, the study was approved with approval number: KAHER/EC/21-22/020.
The consort flow chart representation of materials and methods was shown in Figure 1.
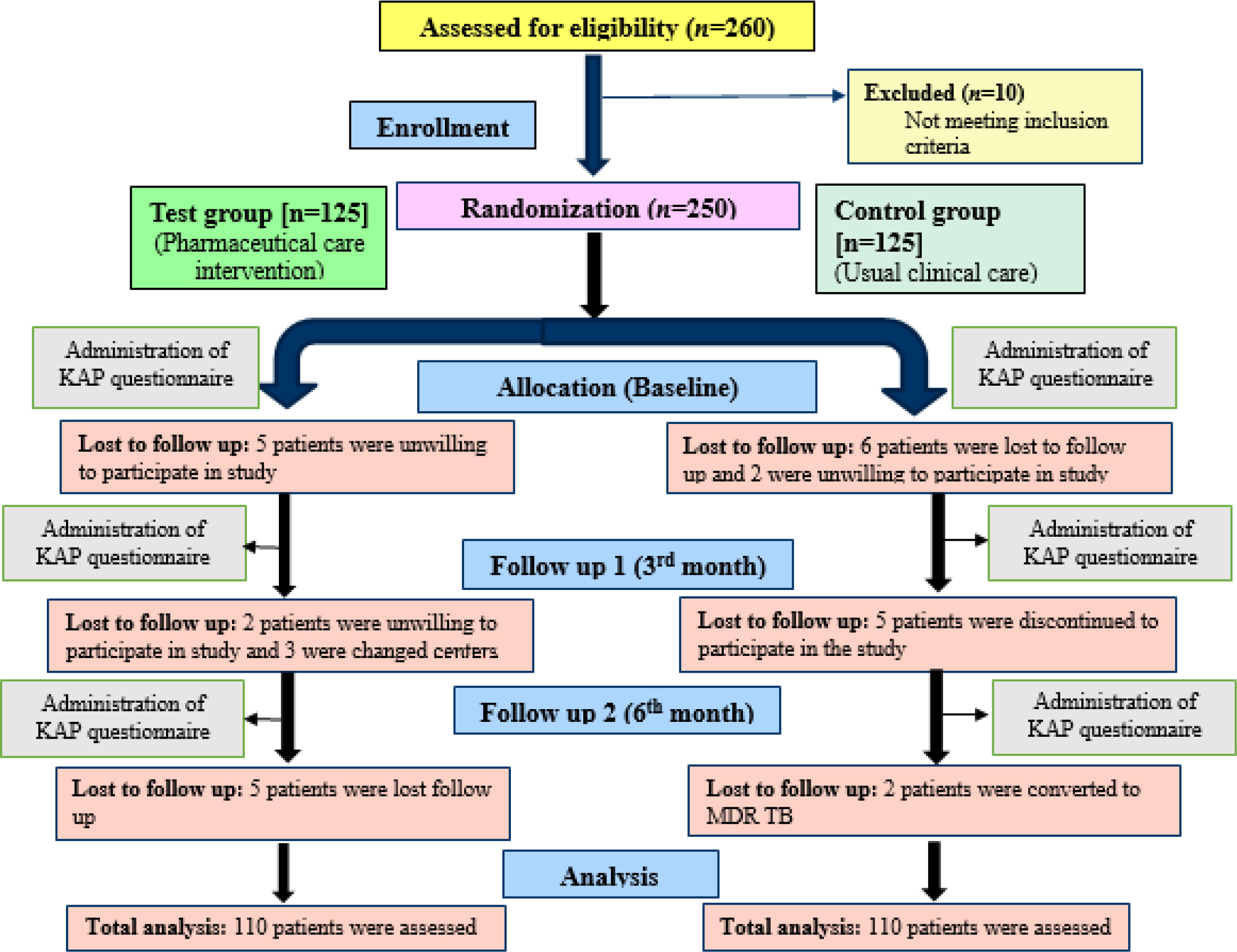
Figure 1:
The consort flow chart representation of materials and methods.
RESULTS
Socio Demographic details
In our study, according to eligibility 250 participants were allocated and were randomised into test and control groups. Almost 20 patients were lost follow up at the end of follow up 2 (6th month). We assessed the KAP of a total number of 220 patients (n=110 test and n=110 control). As far as background information was concerned, majority of the patients were males in both test and control (53.64% in test and 55.45% in control) and majority belonged to the 26-35 years of age group (57.27% in test and 60% in control). Around 83.64% of the patients in both groups were literate and most of them were living in urban residential area compared to rural area in both groups. The marital status was found that majority of them got married (70% in test and 78.18% in control). The socioeconomic status of the patients found that majority were belong to lower middle (31.82% in test and 39.09% in control) followed by upper lower and upper middle-class groups. Most of the patients who were newly diagnosed for TB were taking ATT medication (59.09% in test and 55.45% in control). The social history of the patients found that most of them were Non-alcoholic or smokers (45.45% in test and 50% in control) but there were few smokers (21.82% in test and 23.64% in control) and smokeless tobacco chewing (23.64% in test and 17.27% in control). Majority of the patients were not having any comorbidities only few of them had hypertension (5.45% in control and test) and diabetes (2.73% in test and 3.64% in control) [Table 1].
| Socio-demographic profile | Test (n=110) | (%) | Control (n =110) | (%) |
|---|---|---|---|---|
| Age groups | ||||
| 15-25 | 13 | (11.82) | 11 | (10.00) |
| 26-35 | 63 | (57.27) | 66 | (60.00) |
| 36-45 | 34 | (30.91) | 33 | (30.00) |
| Gender | ||||
| Female | 51 | (46.36) | 49 | (44.55) |
| Male | 59 | (53.64) | 61 | (55.45) |
| Literacy | ||||
| Illiterate | 18 | (16.36) | 18 | (16.36) |
| Literate | 92 | (83.64) | 92 | (83.64) |
| Residency | ||||
| Rural | 52 | (47.27) | 49 | (44.55) |
| Urban | 58 | (52.73) | 61 | (55.45) |
| Marital status | ||||
| Unmarried | 33 | (30.00) | 24 | (21.82) |
| Married | 77 | (70.00) | 86 | (78.18) |
| Socioeconomic Status | ||||
| Upper | 3 | (2.73) | 4 | (3.64) |
| Upper middle | 23 | (20.91) | 16 | (14.55) |
| Lower middle | 35 | (31.82) | 43 | (39.09) |
| Upper lower | 35 | (31.82) | 29 | (26.36) |
| Lower | 14 | (12.73) | 18 | (16.36) |
| TB drug treatment | ||||
| FDC | 45 | (40.91) | 49 | (44.55) |
| ATT | 65 | (59.09) | 61 | (55.45) |
| Social History | ||||
| Smoker | 24 | (21.82) | 26 | (23.64) |
| Smokeless tobacco | 26 | (23.64) | 19 | (17.27) |
| Alcohol | 0 | (0.00) | 3 | (2.73) |
| Alcoholic with smoking | 10 | (9.09) | 7 | (6.36) |
| Non-alcoholic/smoker | 50 | (45.45) | 55 | (50.00) |
| Comorbidities | ||||
| Hypertension | 6 | (5.45) | 6 | (5.45) |
| Diabetes | 3 | (2.73) | 4 | (3.64) |
| No comorbidities | 101 | (91.82) | 100 | (90.91) |
| Total | 110 | 100.0 | 110 | 100.0 |
Health-Seeking behaviour
Regarding health seeking behaviour we assessed that about 97.27% of the patients in both test and control group patients that they usually go to private clinic whenever they feel sick or to treat a general health problem and only 2.73% patients of both groups prefer for government clinic or hospital. About 84.55% in both groups at once in a month generally seek health care at a clinic or hospital, 14.55% in both groups the patients seek at least twice a year or more to the healthcare clinic or hospital followed by only 0.91% patients in both groups seeks once per year to the healthcare clinic or hospital. The comparison of both control and test groups with Health-seeking behaviour of TB patients was mentioned at Table 2.
| Health-seeking behaviour | Control group | % | Test group | % | Total | % |
|---|---|---|---|---|---|---|
| Where do you usually go if you are sick, or to treat a general health problem? | ||||||
| Private clinic | 107 | 97.27 | 107 | 97.27 | 214 | 97.27 |
| Government clinic or hospital | 3 | 2.73 | 3 | 2.73 | 6 | 2.73 |
| How often do you generally seek health care at a clinic or hospital? | ||||||
| Once in a month. | 93 | 84.55 | 93 | 84.55 | 186 | 84.55 |
| Twice a year or more. | 16 | 14.55 | 16 | 14.55 | 32 | 14.55 |
| Once per year. | 1 | 0.91 | 1 | 0.91 | 2 | 0.91 |
| Total | 110 | 100.0 | 110 | 100.0 | 220 | 100.0 |
TB knowledge and awareness
On assessment and evaluation of knowledge and awareness on TB, patients were interviewed about seriousness of the disease, signs and symptoms, TB transmission, prevention, and occurrence among all age groups. The questionnaire administered in three treatment times i.e., baseline, follow up 1 and follow up 2. By using independent t test, at baseline both control and test groups has shown low knowledge and awareness, in which control group mean score 3.35±0.92 and test group mean score 3.55±1.55 with t-value -1.1104 and p-value 0.2681. In follow-up 1 control group mean score 5.24±0.99 and test group mean score 4.23±1.00 with t-value 7.5326 and p-value 0.0001. In follow-up 2 controls group mean score 7.10±1.10 and test group mean score 9.75±0.98 with t-value -18.9101 and p-value 0.0001 which had shown highly significant improvement [Figure 2].

Figure 2:
Comparison of control group and test group with TB knowledge and awareness scores at different treatment times.
TB attitude and Stigma
On assessment and evaluation of attitude and stigma towards TB, patients were interviewed about ATT therapy, reporting side effects, continuation of anti TB treatment when side effects occur, disclosing condition to family members and continuation of anti TB treatment when signs and symptoms were reduced. By using independent t test, at baseline both control and test groups has shown low attitude and stigma, in which control group mean score 2.72±1.44 and test group mean score 2.72±1.44 with t-value 0.0 and p-value 1.0. In follow-up 1 control group mean score 7.73±1.31 and test group mean score 9.40±1.10 with t-value -10.2356 and p-value 0.0001. In follow-up 2 controls group mean score 12.73±1.31 and test group mean score 18.22±1.07 with t-value -34.0073 and p-value 0.0001 which had shown highly significant improvement [Figure 3].
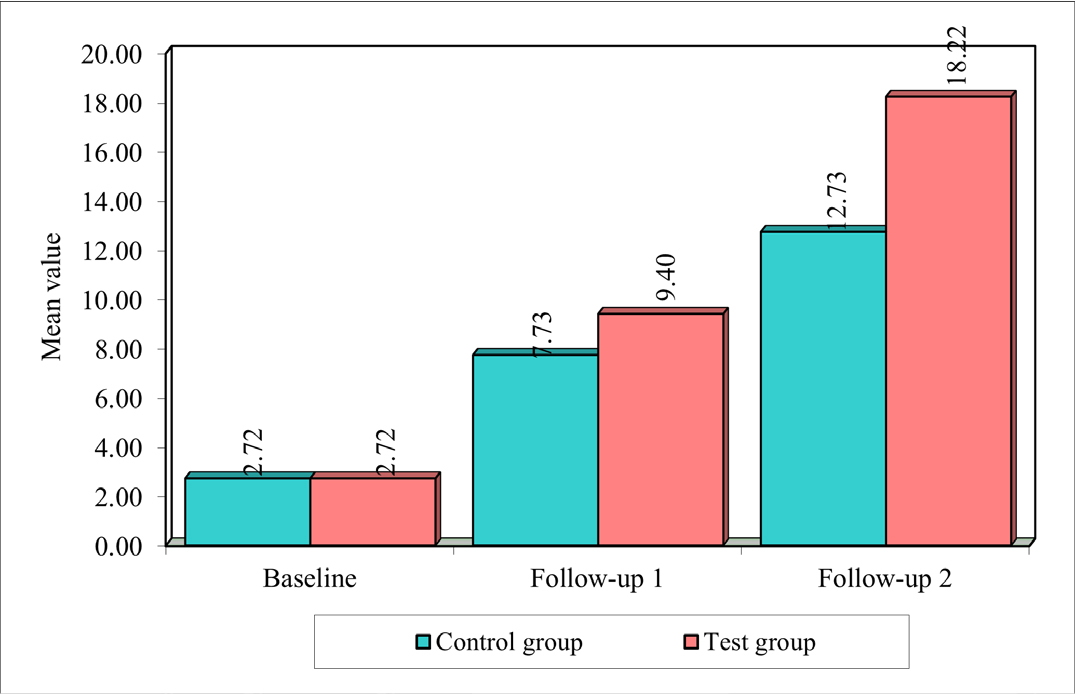
Figure 3:
Comparison of control group and test group with TB attitude and stigma scores at different treatment times.
Perception on TB
On assessment and evaluation of perception towards TB, patients were interviewed about cure, treatment and diagnosis expense, mental stability, sharing TB related problems and information about TB. By using independent t test, at baseline both control and test groups has shown low perception towards TB, in which control group mean score 2.80±1.43 and test group mean score 2.80±1.43 with t-value 0.0 and p-value 1.0. In follow-up 1 control group mean score 3.24±1.45 and test group mean score 2.39±1.82 with t-value 3.8176 and p-value 0.0001. In follow-up 2 controls group mean score 8.07±1.39 and test group mean score 9.85±0.76 with t-value -11.7635 and p-value 0.0001 which had shown highly significant improvement [Figure 4].
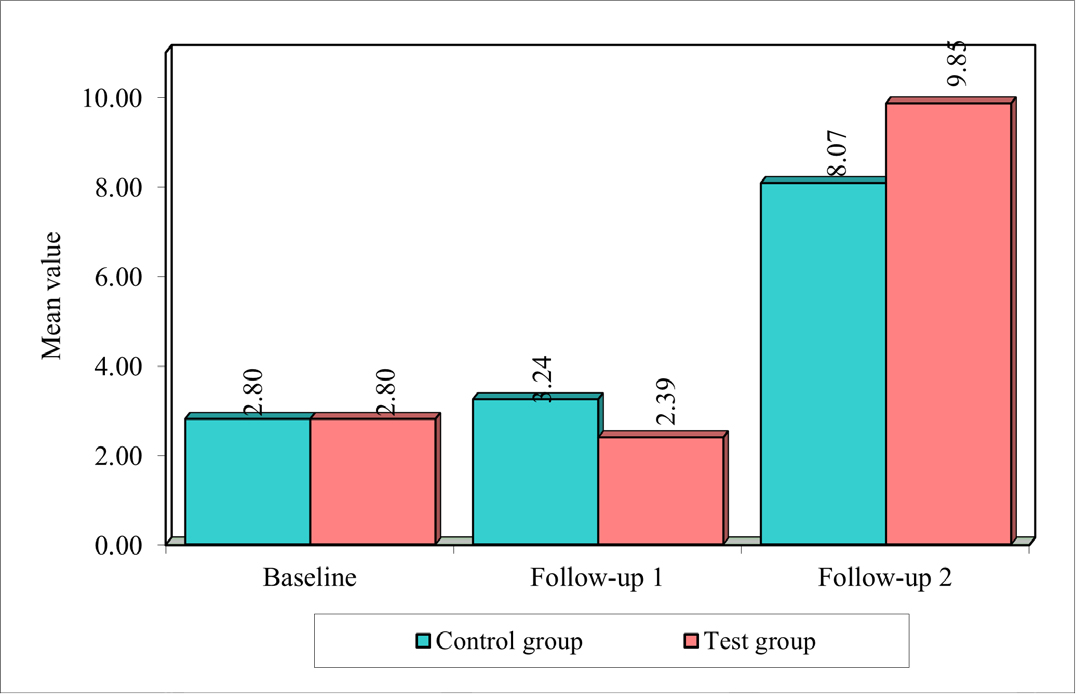
Figure 4:
Comparison of control group and test group with TB Perception scores at different treatment times.
DISCUSSION
At present, clinical pharmacists are most accessible primary healthcare providers in India. Despite the addition of pharmacists in Public-Private Partnership programme under NTEP in India, for being a DOT provider, case finder, counsellor, the awareness and training the pharmacist by central TB center was found inadequate in India.20 The NTEP program provides effective ways to establish the link between disease transmission and infection to initiate TB prophylaxis. Training and education interventions delivered by pharmacists have been evaluated in other countries with high TB burdens and suggest that increased knowledge about TB can change the way High-risk groups approach TB prevention.21
In our study, males were outnumbered than females by constituting more than 50% of the total sample among both test and control. The maximum number of participants were at the working age group 26-35 (57.27% in test and 60% in control). Similar results were reported by Vani et al., (2015) marking a higher incidence rate of TB from 25 to 35 years of age, the rate gradually decreases.22 In our study most of the patients of about 97.27% approached the private health facility for their tuberculosis symptoms. Similar study conducted by Uplekar et al. found that in the Pune city, 60% of individuals with chest symptoms first approached a private provider and in another study by the same author, it was found to be 86%.23,24
In our study, while assessing TB knowledge and awareness at baseline we found that only few participants knew that a seriousness of the TB disease, only few knew that cough was the mode of transmission and were unknown of TB occurrence among different age groups but after pharmacist intervention we found significant improvement among test group patients. In a study by Sabir et al. in Rawalpindi, it was found that the participants had little known knowledge about the causes of TB and the mode of transmission.25 The reason for this large difference may be because our study was carried out in both urban and rural areas. However, another study conducted in Sudan rural area by Mohamed et al. showed that only 1.9% of the participants knew the cause of TB.26
In our study we found that more than a quarter of participants had low attitude and found high stigma regarding TB in the baseline and after pharmacist intervention we found significant improvement in test group patients. In a study conducted by Mweemba et al. in Zambia showed that 80% of participants had a positive attitude towards TB.27 Our study also observed that 49.1% of the participants agreed to disclose TB to family members and isolate TB patients. This shows that TB patients are still discriminated against in our society. Although the attitude to continue taking anti-TB drugs even when symptoms declined was good, only few of them reports the side effects.
In our study while we found, most of them have negative perception opinion in curing and were thought expensive with treatment and diagnosis available in India. According to Central TB division, it was reported that 80-85% of patients were successfully treated; all diagnostic tests and treatment expenses were available free under NTEP programme.28 This extension gap in attitude and perception can be reduced with appropriate interventions and equitable distribution of health services in all regions. Several studies have shown that knowledge about TB increases by conducting awareness interventional programs.29–31 Hence, we believe the role of clinical pharmacist plays an important role with NTEP programme in providing and educating the TB patients to know about their disease condition.
CONCLUSION
We conclude majority of the patients in both control and test groups were having lack of knowledge and awareness, low attitude and perception on TB at the baseline. After intervention from a clinical pharmacist and usual care from health care team, we found significant improvement among TB patients. Test group patients have shown greater improvement than control group. It was shown that clinical pharmacist adequate counselling and education of patients Played an important role aspect in reducing the stigma, the impact of social consequences of TB and completion of anti TB treatment within duration of period. Thus, the clinical pharmacists have a significant role in the national strategy plan in elimination of TB from India by 2025.
Cite this article
Raja BY, Ganachari MS, Assessment and Evaluation of Knowledge, Attitude and Perception among Pulmonary Tuberculosis Patients in Belagavi Region. J Young Pharm. 2024;16(1):95-101.
LIMITATIONS
The findings are limited to only one tertiary care hospital and four PHC centres only in Belagavi. So, the results cannot be fully extrapolated for general population. Moreover, patients attending government hospitals are expected to have a relatively greater awareness on health issues.
FINANCIAL SUPPORT AND SPONSORSHIP
Ministry of Health and Family Welfare, Government of Karnataka.
ABBREVIATIONS
| TB | Tuberculosis |
|---|---|
| WHO | World Health Organisation |
| MDR-TB | Multi drug-resistance tuberculosis |
| HIV | Human immunodeficiency virus |
| AIDs | Acquired immunodeficiency syndrome |
| KAP | Knowledge, attitude and perception |
| RNTCP | Revised National Tuberculosis Control Programme |
| NTEP | National Tuberculosis Elimination Program |
| IEC | Institutional Ethical Clearance |
| PHC | Primary Health Care centre |
| PILs | Patient Information Leaflets |
| FRE | Flesch Reading Ease |
| BALD | Baker Able Leaflet Design |
| ATT | Antitubercular treatment |
| FDC | Fixed Dose Combination therapy |
| ICF | Informed consent forms |
References
- Shrinivasan R, Rane S, Pai M. India’s syndemic of tuberculosis and COVID-19. BMJ Glob Health. 2020;5(11):e003979 [PubMed] | [CrossRef] | [Google Scholar]
- WHO. Global tuberculosis control: WHO report. 2011 Available fromhttp://whqlibdo c.who;2011.int/publications/2011/9789241564380_eng.pdf
- Tiemersma EW, van der Werf MJ, Borgdorff MW, Williams BG, Nagelkerke NJ. Natural history of tuberculosis: duration and fatality of untreated pulmonary tuberculosis in HIV negative patients: a systematic review. PLOS ONE. 2011;6(4):e17601 [PubMed] | [CrossRef] | [Google Scholar]
- Khanna A, Saha R, Ahmad N. National TB elimination programme – what has changed. Indian J Med Microbiol. 2023;42:103-7. [PubMed] | [CrossRef] | [Google Scholar]
- Sachdeva KS, Kumar A, Dewan P, Kumar A, Satyanarayana S. New vision for Revised National Tuberculosis Control Programme (RNTCP): universal access – “reaching the un-reached”. Indian J Med Res. 2012;135(5):690-4. [PubMed] | [Google Scholar]
- Otu AA. Is the directly observed therapy short course (DOTS) an effective strategy for tuberculosis control in a developing country?. Asian Pac J Trop Dis. 2013;3(3):227-31. [CrossRef] | [Google Scholar]
- Kempinski R, Krasnik A. Prevention of arteriosclerotic heart disease. An epidemiological study of knowledge, attitudes and practices in a community in Israel. Ugeskr Laeger. 1974;136(34):1931-8. [PubMed] | [Google Scholar]
- Suleiman MM, Sahal N, Sodemann M, Elsony A, Aro AR. Tuberculosis awareness in Gezira, Sudan: knowledge, attitude and practice case-control survey. East Mediterr Health J. 2014;20(2):120-9. [PubMed] | [CrossRef] | [Google Scholar]
- Khalil A, Abdalrahim M. Knowledge, attitudes, and practices towards prevention and early detection of chronic kidney disease. Int Nurs Rev. 2014;61(2):237-45. [PubMed] | [CrossRef] | [Google Scholar]
- Matsumoto-Takahashi EL, Tongol-Rivera P, Villacorte EA, Angluben RU, Jimba M, Kano S, et al. Patient knowledge on malaria symptoms is a key to promoting universal access of patients to effective malaria treatment in Palawan, the Philippines. PLOS ONE. 2015;10(6):e0127858 [PubMed] | [CrossRef] | [Google Scholar]
- Masud R, Abu S, Reazul K, Nurul I. Assessment of knowledge regarding TB among non-medical university students in Bangladesh: a cross sectional study. BMC Public Health. 2015;15:716 [PubMed] | [CrossRef] | [Google Scholar]
- Bansal AB, Pakhare AP, Kapoor N, Mehrotra R, Kokane AM. Knowledge, attitude, and practices related to cervical cancer among adult women: a hospital-based cross-sectional study. J Nat Sci Biol Med. 2015;6(2):324-8. [PubMed] | [CrossRef] | [Google Scholar]
- Terán Calderón C, Gorena Urizar D, González Blázquez C, Alejos Ferreras B, Ramírez Rubio O, Bolumar Montrull F, et al. Knowledge, attitudes and practices on HIV/AIDS and prevalence of HIV in the general population of Sucre, Bolivia. Braz J Infect Dis. 2015;19(4):369-75. [PubMed] | [CrossRef] | [Google Scholar]
- Gimenez-Sanchez F, Butler JC, Jernigan DB, Strausbaugh LJ, Slemp CC, Perilla MJ, et al. Treating cardiovascular disease with antimicrobial agents: a survey of knowledge, attitudes, and practices among physicians in the United States. Clin Infect Dis. 2001;33(2):171-6. [PubMed] | [CrossRef] | [Google Scholar]
- Deshpande PR, Vantipalli R, Chaitanya Lakshmi CH, Rao EJ, Regmi B, Ahad A, et al. Clinical pharmacists: the major support to Indian healthcare system in near future. J Pharm Bioallied Sci. 2015;7(3):161-74. [PubMed] | [CrossRef] | [Google Scholar]
- Gebreweld FH, Kifle MM, Gebremicheal FE, Simel LL, Gezae MM, Ghebreyesus SS, et al. Factors influencing adherence to tuberculosis treatment in Asmara, Eritrea: a qualitative study. J Health Popul Nutr. 2018;37(1):1 [PubMed] | [CrossRef] | [Google Scholar]
- Thakur G, Thakur S, Thakur H. Status and challenges for tuberculosis control in India – Stakeholders’ perspective. Indian J Tuberc. 2021;68(3):334-9. [PubMed] | [CrossRef] | [Google Scholar]
- Iskandar D, Suryanegara FDA, van Boven JFM, Postma MJ. Clinical pharmacy services for tuberculosis management: a systematic review. Front Pharmacol. 2023;14:1186905 [PubMed] | [CrossRef] | [Google Scholar]
- World Health Organization. A guide to developing knowledge, attitude, and practice surveys Suiza. WHO. 2008 [PubMed] | [CrossRef] | [Google Scholar]
- Suseela RP, Shannawaz M. Engaging the Private Health Service Delivery Sector for TB Care in India-miles to Go!. Trop Med Infect Dis. 2023;8(5):265 [PubMed] | [CrossRef] | [Google Scholar]
- Zaeh S, Kempker R, Stenehjem E, Blumberg HM, Temesgen O, Ofotokun I, et al. Improving tuberculosis screening and isoniazid preventive therapy in an HIV clinic in Addis Ababa, Ethiopia. Int J Tuberc Lung Dis. 2013;17(11):1396-401. [PubMed] | [CrossRef] | [Google Scholar]
- Vani M, Usha M. Knowledge and behaviour among tuberculosis patients of Dharwad, Karnataka. The Pharm Innov J. 2019;8(2):218-21. [PubMed] | [CrossRef] | [Google Scholar]
- Uplekar M, Rangan S. Tackling TB: the search for solutions: Foundation for Research in Community Health. 1996 [PubMed] | [CrossRef] | [Google Scholar]
- Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis. 1998;2(4):324-9. [PubMed] | [Google Scholar]
- Sabir SA, Naseem U, Abideen Z, Chisti MJ. Assessment of “tuberculosis preventive knowledge” in persons taking care of TB-patients. J Rawal Coll. 2012;16(1):62-4. [PubMed] | [Google Scholar]
- Mohamed AI, Yousif MA, Ottoa P, Bayoumi A. Knowledge of tuberculosis: a survey among tuberculosis patients in Omdurman, Sudan. Sudanese J Public Health. 2007;2(1):21-8. [PubMed] | [Google Scholar]
- Mweemba P, Haruzivishe C, Siziya S, Chipimo P, Cristenson K, Johansson E, et al. Knowledge, attitudes and compliance with tuberculosis treatment, Lusaka, Zambia. Med J Zamb. 2008;35(4) [CrossRef] | [Google Scholar]
- India TB. Central TB division. 2017 Available fromhttp://www.tbcindia.nic.in/pdf/TB
- Carey JW, Oxtoby MJ, Nguyen LP, Huynh V, Morgan M, Jeffery M, et al. Tuberculosis beliefs among recent Vietnamese refugees in New York state. Public Health Rep. 1997;112(1):66-72. [PubMed] | [Google Scholar]
- Dick J, Lombard C. Shared vision-a health education project designed to enhance adherence to anti-tuberculosis treatment. Int J Tuberc Lung Dis. 1997;1(2):181-6. [PubMed] | [Google Scholar]
- Hoa NP, Thorson AE, Long NH, Diwan VK. Knowledge of tuberculosis and associated health-seeking behaviour among rural Vietnamese adults with a cough for at least three weeks. Scand J Public Health Suppl. 2003;62:59-65. [PubMed] | [CrossRef] | [Google Scholar]
