ABSTRACT
ABSTRACT
Background
Burning Mouth Syndrome (BMS) is a type of persistent, debilitating orofacial discomfort that is characterized by an oral mucosal burning sensation that does not occur in the presence of any specific oral disease. Aim of this study was to evaluate the clinical features and medication for burning mouth condition.
Materials and Methods
We examined the DIAS case file from June 2022 to March 2023, during which 50 samples were identified. Data were gathered using a specific table designed for data collection and a customized examination form. Chi square test and descriptive statistics were used to analyse the data. p >0.05, statistically significant.
Results
From the study, around (38.8%) of the participants who had burning mouth syndrome are due to anxiety followed by dryness and irritation (22.2%). Current research shows that around 78% of the participants are female. Majority of the females had anxiety as the main etiological factor compared to males. Pearson chi square-10.68, p >0.016, statistically significant. Majority of the patients used Benzydamine HCl as the topical application (66%) for BMS.
Conclusion
Current study proves that, majority of the burning mouth syndrome patients are females and the most common etiological factor has been found to be anxiety. Better management can be provided to patients only when the etiology is understood properly and diagnosed in a right way.
INTRODUCTION
According to the International Association for the Study of Pain, this syndrome is characterized by ““burning pain with normal signs and laboratory results in the tongue or other oral mucous membrane” 2 hr per day lasting at least 4-6 months”.1 A persistent oral burning sensation or dysesthesia without aberrant oral mucosal findings is the hallmark of BMS, is a persistent pain condition of the orofacial region.2 BMS can be divided into primary and secondary subtypes according to its etiology. The development of oral burning sensation (secondary type of BMS) was linked to a number of systemic diseases like diabetes3 and oral mucosal lesions including oral lichen planus,4 oral candidiasis,5 and others. The diagnosis of the true main type of BMS can be determined when these etiological factors have been ruled out.6 Patients with Burning Mouth Syndrome (BMS) frequently report experiencing stinging or burning discomfort on their tongue, lips, palatal region, and other oral mucosa that chiefly affects middle or old age women. Dry mouth (xerostomia), a change in taste (dysgeusia), and oral paraesthesia are accompanying symptoms.7 About 0.7% and 15% of the general population have BMS, and the ratio of male to female varies from 1:3 to 1:16. The severity of the symptom’s peaks later in the afternoon and ends in the evening, rarely interfering with the patient’s sleep. They also change depending on the type of food consumed and the patient’s emotional condition.8 The predominant symptom of BMS is still oral burning discomfort. The location of pain frequently involves multiple sites and is not pathognomonic. Some people have low quality of life, somatization, fear, depression, and/or a loss of social desire when pain changes their sleep patterns.9 There is no corrective regimen for BMS therapy. Patients are guided through a variety of therapy, with results that range from tongue guards to prescription medications that aren’t always suitable.10 The same treatments are not effective for all BMS patients since the underlying pathophysiology of BMS neuropathic pathways is complex and differs according to the patient.11 There is evidence that topical and systemic medication, nutritional supplements, low-level laser therapy, behavioural interventions, and topical and systemic pharmacotherapy may be useful in managing pain and other symptoms related to BMS. However, none of these treatments have demonstrated a clear response.12 Hence, the study’s aim was to evaluate the clinical characteristics and pharmacotherapy in burning mouth syndrome patients.
MATERIALS AND METHODS
Saveetha Dental College and Hospitals, Chennai, India, was the site of the current study. Patients with a similar ethnic background and geographic origin made up the data that was currently available. Digital case records of 50 patients who presented to the hospital were used to conduct the retrospective study. The hospital’s Scientific Review Board gave its approval for the study’s ethical conduct. SDC/SIHEC/2021/DIASDATA/0619-0320 is the ethical approval number for this investigation. Review and data extraction were done on 50 patients’ records-11 men and 39 women. In the time frame specified, every patient with burning mouth symptoms was examined. To reduce sample bias, we included only pertinent data. A straightforward random sampling procedure was used. Data cross-checking was done to look for errors. Reviewing patients’ records for burning mouth syndrome was done in order to collect data, which was then assessed between June 2022 and March 2023. Data on the burning mouth syndrome were gathered and categorized based on factors including age, gender, etiology, etc. Statistical Package for Social Sciences for Windows, version 20.0 (SPSS Inc., Vancouver style), was used to tabulate and analyse the collected data, and it produced the desired findings. Percentage and frequency were used to express categorical variables. To examine the relationship between categorical variables, the chi square test was applied. Age, gender, and other independent and dependent variables were tested using chi square. Pearson chi square test was used for the statistical analysis. Statistical significance was defined as a p value 0.05.
RESULTS
Figure 1 represents the medication used by the patients for burning mouth syndrome. Majority of the patients have used Benzydamine HCl as the topical application (66%). Figure 2 shows the duration of illness. Majority around 44.4% of the participants have been under BMS for around 4-6 months. Figure 3 indicates the pain intensity undergone by the patients. Around 44.4% of the patients have undergone intermittent pain followed by constant pain 33.3%. The correlation between etiology and gender was shown in Figure 4. Compared to men, the majority of the females had anxiety as the primary etiological cause. Chi square analysis was performed. The results of the chi square analysis (Pearson chi square-15.62) revealed a p value of 0.016 0.05, which is statistically significant. The relationship between age and etiology was seen in Figure 5. Anxiety was the primary etiological factor in the majority of individuals between the ages of 18 and 30 years. Anxiety was the primary etiological factor in the majority of individuals between the ages of 18 and 30 years. It was determined by chi square analysis (Pearson chi square-10.68) that the p value was 0.345>0.05, which is statistically insignificant. The correlation between clinical results and patient gender was shown in Figure 6. As clinical findings in burning mouth syndrome, more females than males exhibited altered tastes and a burning sensation. It was determined that the p value for the chi square (Pearson chi square-11.21) was 0.061> 0.05, which was statistically insignificant.

Figure 1:
Bar graph shows the medication used by the participants for burning mouth syndrome. Medication was represented on the X axis, and the percentage of patients who have burning mouth syndrome is shown on the Y axis. Benzydamine HCl (Silver) was used to treat the majority of patients with burning mouth syndrome, compared to lidocaine gel (Grey), which was used to treat 33.3% of them.

Figure 2:
Bar graph depicts the duration of illness. The percentage of patients having burning mouth syndrome was shown on the Y axis, while the X axis shows the duration that the illness has lasted for each patient. The majority of patients with burning mouth syndrome had 4-6 month illness duration (Teal) compared to less than 3 months (Navy blue) (44.4%, 22.2%).

Figure 3:
Bar graph depicts the participants’ level of pain. The X axis shows the degree of pain, while the Y axis shows the proportion of individuals having burning mouth syndrome. Most patients with burning mouth syndrome experienced sporadic pain (maroon), which made up 44.4% of them, as compared to chronic discomfort (turquoise blue), which made up 33.3%.

Figure 4:
Bar graph shows the relationship between the etiology and gender patients with burning mouth syndrome, X axis according to their etiology, and on the Y axis according to their gender. Males are represented by Blue, while females by Green. Compared to men, the majority of the females had anxiety as the primary etiological cause. The results of the chi square analysis (Pearson chi square-15.62) revealed a p value of 0.016 0.05, which is statistically significant.
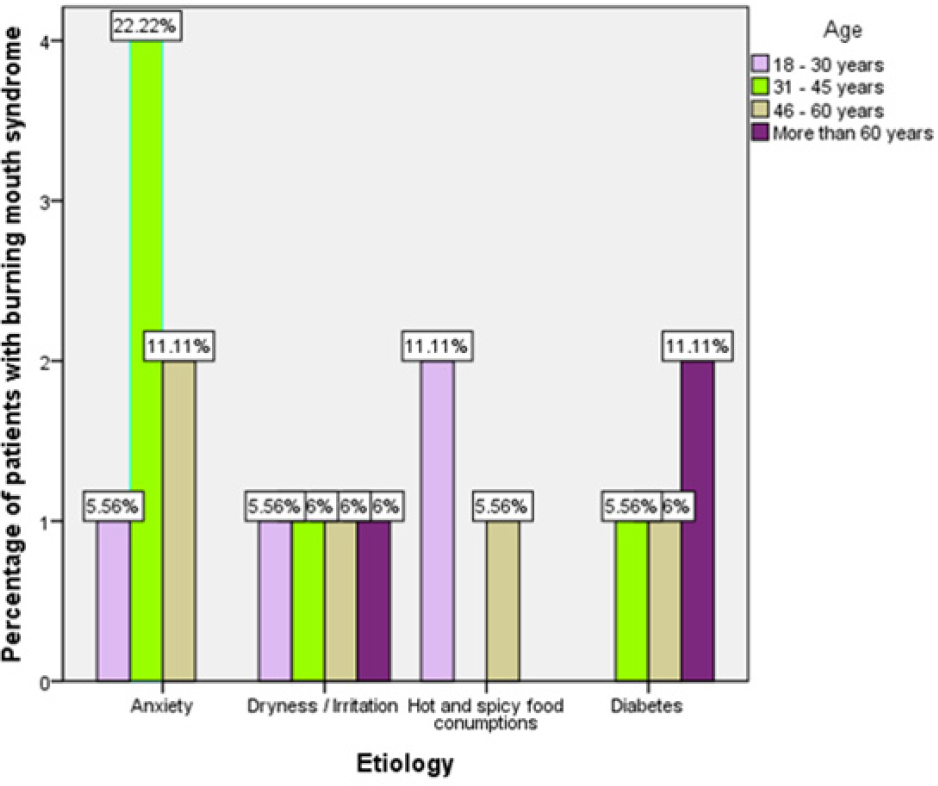
Figure 5:
Bar graph depicts the association between age and the etiology of burning mouth syndrome patients. The etiology was shown on the X axis, while age is shown on the Y axis. Lavender stands for ages 18 to 30, lime for ages 31 to 45, beige for ages 46 to 60, and violet for ages over 60. Anxiety was the primary etiological factor in the majority of individuals between the ages of 18 and 30. It was determined by chi square analysis (Pearson chi square-10.68) that the p value was 0.345>0.05, which is statistically insignificant.
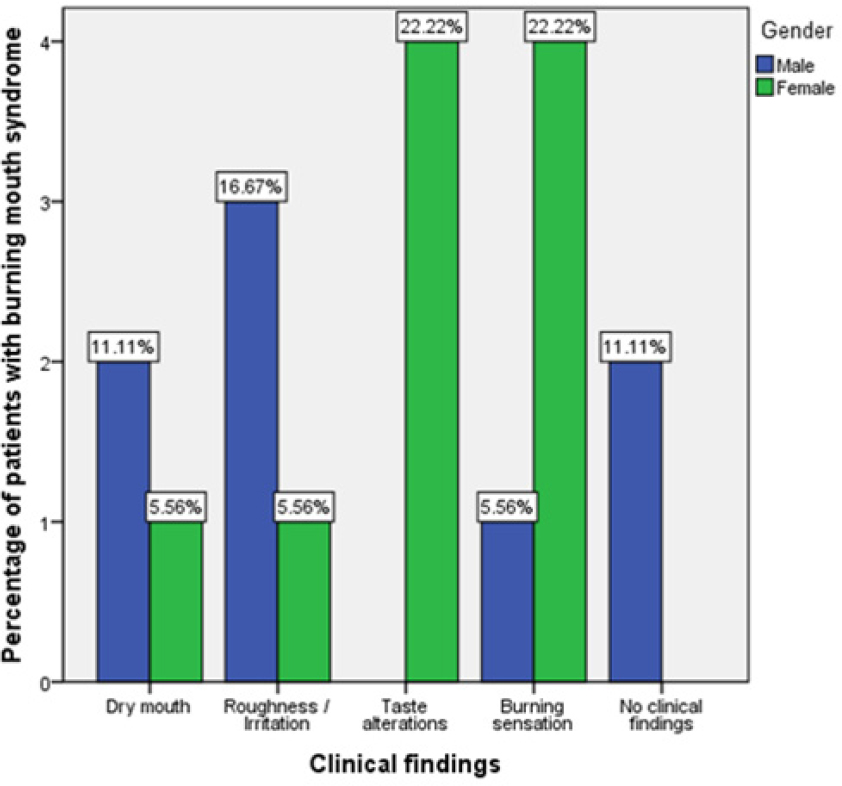
Figure 6:
This bar graph shows the relationship between the patients’ clinical outcomes and gender. While the gender was shown by the Y axis, clinical data are represented by the X axis. Male is symbolized by Blue, and female by Green. In contrast to males, the majority of females with burning mouth syndrome exhibited altered taste and a burning sensation. An analysis of the chi square (Pearson chi square-11.21) revealed a p value of 0.061>0.05, which is statistically insignificant.
DISCUSSION
Patients with burning mouth syndrome frequently experience pain as a result of this illness. BMS frequently has a complex etiology with multiple contributing factors, and its underlying cause may even be idiopathic. It seems like BMS has a complicated etiopathogenesis.13
According to our study, patients between the ages of 31 and 45 are the most frequently affected by burning mouth syndrome, in contrast to Lim et al.’s study, which found that the mean age was 63 years and that the range of ages from 23 to 89 years.14 Burning mouth syndrome, which is caused by hormonal changes or physiological abnormalities, most frequently affects middle-aged and elderly women. With a mean age of about 60 years, menopausal and postmenopausal women experience BMD significantly more frequently than do men.15 The results of our investigation show a correlation between age and etiology; nevertheless, the chi-square value, which is 0.345>0.05, is not statistically significant. Anxiety was the predominant etiological factor in the majority of patients between the ages of 18 and 30. Our analysis demonstrated that approximately 78% of the participants are females, which was consistent with a study by Khawaja et al. who found that patients with BMS had a roughly 1:4 male to female ratio.16 According to the results of the current study, female patients are the most frequent and vulnerable groups for developing burning mouth syndrome. Compared to men, the majority of the females had anxiety as the primary etiological cause. The results of the chi square analysis (Pearson chi square-15.62) revealed a p value of 0.016 0.05, which is statistically significant.
According to our study, which included 39% of the participants, anxiety was the most frequent cause of the burning mouth condition, which was consistent with research done by Van der Wal.17 According to the results of the previous study, patients had mild to severe depression, suggesting that depression and anxiety are common symptoms in postmenopausal women.18 According to the research done by A. Saerdella et al. in 2007, the majority of the participants-roughly 67%-had Benzydamine HCL prescribed to them. This medication has been shown to be beneficial in treating burning mouth syndrome.19
It has been established that the burning mouth syndrome illness lasts an average of 4-6 months (44%), with the average length of time being 6 months. Our research showed that 44% of the individuals experienced intermittent discomfort, which was followed by persistent, throbbing pain, which was consistent with the 2011 study by Netto et al.20 According to our research, patients with burning mouth syndrome experience symptoms that are either burning or painful. Compared to men, the majority of female patients with burning mouth syndrome reported taste changes and burning sensations. p value was determined after doing a chi square (Pearson chi square-11.21).
CONCLUSION
Current study has proven that, majority of the patients with burning mouth syndrome are females and the most common etiological factor has been found to be anxiety. Majority of the patients from our study has experienced intermittent pain and burning sensation as clinical findings. It was difficult for dental health care specialists to diagnose and treat BMS. For better care, a detailed knowledge of the psychological effects and etiology of this condition was needed along with novel pharmacological approaches.
Cite this article
Dharman S, Abitha TS. Assessment of Clinical Characteristics and Pharmacotherapy in Burning Mouth Syndrome Patients. J Young Pharm. 2023;15(4):730-3.
ACKNOWLEDGEMENT
The authors would thank all the participants for their valuable support and authors thank the dental institution for the support to conduct.
ABBREVIATIONS
| BMS | Burning Mouth Syndrome |
|---|---|
| IHEC | Institutional Human Ethical Committee |
| DIAS | Digital Information Archiving Software |
| SPSS | Statistical Package for Social Sciences for Windows |
References
- Grinspan D, Fernández Blanco Gr, Angel Allevato MI, Stengel FM. Burning mouth syndrome. Int J Dermatol. 1995;34(7):483-7. [PubMed] | [CrossRef] | [Google Scholar]
- Klasser GD, Grushka M, Su N. Burning mouth syndrome. Oral Maxillofacial Surg Clin N Am. 2016;28(3):381-96. [PubMed] | [CrossRef] | [Google Scholar]
- Prasath R, Sinduja P. Knowledge And Awareness on Various Treatment Modalities of Diabetes Mellitus-A Observational Survey. J Educ Teach Train. 2022;13(6):190-8. [CrossRef] | [Google Scholar]
- Dharman S, Ravinthar K. Role of Curcumin in Alleviating Symptomatic Oral Lichen Planus: A Systematic Review. J Clin Diagnostic Res. 2020;14(2):1-6. [CrossRef] | [Google Scholar]
- Divyadharsini V, UmaMaheswari TN, Rajeshkumar S. Comparison of antifungal activity of probiotics, coconut oil and clotrimazole on Candida albicans-An In vitro study. J Indian Acad Oral Med Radiol. 2022;34(4):385-9. [CrossRef] | [Google Scholar]
- Kim MJ, Kim J, Kho HS. Comparison of clinical characteristics between burning mouth syndrome patients with bilateral and unilateral symptoms. Int J Oral Maxillofac Surg. 2020;49(1):38-43. [PubMed] | [CrossRef] | [Google Scholar]
- Jääskeläinen SK. Is burning mouth syndrome a neuropathic pain condition?. Pain. 2018;159(3):610-3. [PubMed] | [CrossRef] | [Google Scholar]
- McMillan R, Forssell H, Buchanan JA, Glenny AM, Weldon JC, Zakrzewska JM, et al. Interventions for treating burning mouth syndrome. Cochrane Database Syst Rev. 2016;11:1-109. [PubMed] | [CrossRef] | [Google Scholar]
- Antoun Reyad A, Mishriky R, Girgis E. Pharmacological and non-pharmacological management of burning mouth syndrome: a systematic review. Dent Med Probl. 2020;57(3):295-304. [PubMed] | [CrossRef] | [Google Scholar]
- Carvalho VJ, Gallo CD, Sugaya NN, Domaneschi C. Clinical characteristics and therapeutic response in patients with Burning Mouth Syndrome: accompanying 2 years. Rev Odontol UNESP. 2017;46:45-50. [CrossRef] | [Google Scholar]
- Teruel A, Patel S. Burning mouth syndrome: a review of etiology, diagnosis, and management. General dentistry. 2019;67(2):24-9. [PubMed] | [Google Scholar]
- Miziara I, Chagury A, Vargas C, Freitas L, Mahmoud A. Therapeutic options in idiopathic burning mouth syndrome: literature review. Int Arch Otorhinolaryngol. 2015;19:86-9. [PubMed] | [CrossRef] | [Google Scholar]
- Aravindhan R, Vidyalakshmi S, Kumar MS, Satheesh C, Balasubramanium AM, Prasad VS, et al. Burning mouth syndrome: A review on its diagnostic and therapeutic approach. J Pharm Bioallied Sci. 2014;6(Suppl 1):S21 [PubMed] | [CrossRef] | [Google Scholar]
- Lim BW, Kim HD, Chang JS, Choi IS. Burning Mouth Syndrome: Patient Profiles, Clinical Symptoms, Affecting Associated Factors, and Treatment Responses. Int J Otorhinolaryngol Head Neck Surg. 2018;7(4):237-48. [CrossRef] | [Google Scholar]
- Alsabbagh R, Ouanounou A. Burning Mouth Syndrome: Etiology, clinical presentations, and treatment alternatives. Dent Rev. 2022;2(1):100036 [CrossRef] | [Google Scholar]
- Khawaja SN, Furlan Bavia P, Keith DA. Clinical Characteristics, Treatment Effectiveness, and Predictors of Response to Pharmacotherapeutic Interventions in Burning Mouth Syndrome: A Retrospective Analysis. J Oral Facial Pain Headache. 2020;34(2) [PubMed] | [CrossRef] | [Google Scholar]
- Van der Ploeg HM, Van der Wal N, Eijkman MA, Van der Waal I. Psychological aspects of patients with burning mouth syndrome. Oral Surg Oral Med Oral Radiol. 1987;63(6):664-8. [PubMed] | [CrossRef] | [Google Scholar]
- Baskar K, Dharman S. Evaluation of Calcium and Alkaline Phosphatase in the Salivary Samples of Premenopausal and Postmenopausal Women. Journal of Pharmaceutical Research International. 2020;32(19):157-63. [CrossRef] | [Google Scholar]
- Sardella A, Lodi G, Demarosi F, Uglietti D, Carrassi A. Causative or precipitating aspects of burning mouth syndrome: a case-control study. J Oral Pathol. Med. 2006;35(8):466-71. [PubMed] | [CrossRef] | [Google Scholar]
- Netto FO, Diniz IM, Grossmann SM, de Abreu MH, do Carmo MA, Aguiar MC, et al. Risk factors in burning mouth syndrome: a case-control study based on patient records. Clin. Oral Investig. 2011;15:571-5. [PubMed] | [CrossRef] | [Google Scholar]
